FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Abraxane Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
There is currently no warning information available for this product. We apologize for any inconvenience.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Exjade is indicated for the treatment of chronic iron overload due to blood transfusions (transfusional hemosiderosis) in patients 2 years of age and older. This indication is based on a reduction of liver iron concentrations and serum ferritin levels [see Clinical Studies (14)]. An improvement in survival or disease-related symptoms has not been established [see Indications and Usage (1.3)].
Exjade is indicated for the treatment of chronic iron overload in patients 10 years of age and older with non-transfusion-dependent thalassemia (NTDT) syndromes and with a liver iron concentration (LIC) of at least 5 milligrams of iron per gram of liver dry weight (mg Fe/g dw) and a serum ferritin greater than 300 mcg/L. This indication is based on achievement of an LIC less than 5 mg Fe/g dw [see Clinical Studies (14)]. An improvement in survival or disease-related symptoms has not been established.
Controlled clinical trials of Exjade with myelodysplastic syndromes (MDS) and chronic iron overload due to blood transfusions have not been performed [see Clinical Studies (14)].
The safety and efficacy of Exjade when administered with other iron chelation therapy have not been established.
History
There is currently no drug history available for this drug.
Other Information
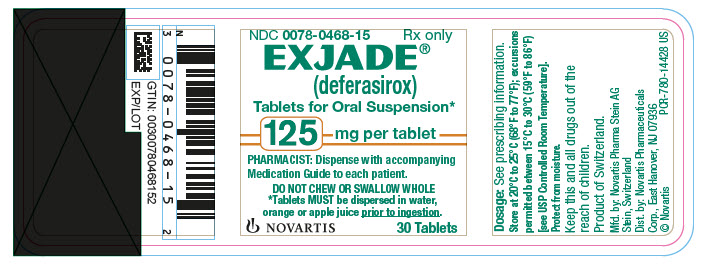
Exjade (deferasirox) is an iron chelating agent. Exjade tablets for oral suspension contain 125 mg, 250 mg, or 500 mg deferasirox. Deferasirox is designated chemically as 4-[3,5-Bis (2-hydroxyphenyl)-1H-1,2,4-triazol-1-yl]-benzoic acid and its structural formula is:
Deferasirox is a white to slightly yellow powder. Its molecular formula is C21H15N3O4 and its molecular weight is 373.4.
Inactive Ingredients: Lactose monohydrate (NF), crospovidone (NF), povidone (K30) (NF), sodium lauryl sulphate (NF), microcrystalline cellulose (NF), silicon dioxide (NF), and magnesium stearate (NF).
Sources
Abraxane Manufacturers
-
Abraxis Bioscience, Llc
![Abraxane (Paclitaxel) Injection, Powder, Lyophilized, For Suspension [Abraxis Bioscience, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Abraxane | Novartis Pharmaceuticals Corporation
![Abraxane (Paclitaxel) Injection, Powder, Lyophilized, For Suspension [Abraxis Bioscience, Llc] Abraxane (Paclitaxel) Injection, Powder, Lyophilized, For Suspension [Abraxis Bioscience, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 Transfusional Iron OverloadExjade therapy should only be considered when a patient has evidence of chronic transfusional iron overload. The evidence should include the transfusion of at least 100 mL/kg of packed red blood cells (e.g., at least 20 units of packed red blood cells for a 40 kg person or more in individuals weighing more than 40 kg), and a serum ferritin consistently greater than 1000 mcg/L.
Prior to starting therapy, obtain:
serum ferritin level baseline serum creatinine in duplicate (due to variations in measurements) and determine the creatinine clearance (Cockcroft-Gault method) [see Dosage and Administration (2.4), Warnings and Precautions (5.1)] serum transaminases and bilirubin [see Dosage and Administration (2.4), Warnings and Precautions (5.2)] baseline auditory and ophthalmic examinations [see Warnings and Precautions (5.9)]The recommended initial dose of Exjade for patients 2 years of age and older is 20 mg per kg body weight orally, once daily. Calculate doses (mg per kg per day) to the nearest whole tablet.
After commencing therapy, monitor serum ferritin monthly and adjust the dose of Exjade, if necessary, every 3-6 months based on serum ferritin trends. Make dose adjustments in steps of 5 or 10 mg per kg and tailor adjustments to the individual patient’s response and therapeutic goals. In patients not adequately controlled with doses of 30 mg per kg (e.g., serum ferritin levels persistently above 2500 mcg/L and not showing a decreasing trend over time), doses of up to 40 mg per kg may be considered. Doses above 40 mg per kg are not recommended.
If the serum ferritin falls consistently below 500 mcg/L, consider temporarily interrupting therapy with Exjade [see Warnings and Precautions (5.10)].
2.2 Iron Overload in Non-Transfusion-Dependent Thalassemia SyndromesExjade therapy should only be considered when a patient with NTDT syndrome has an LIC of at least 5 mg Fe/g dw and a serum ferritin greater than 300 mcg/L.
Prior to starting therapy, obtain:
LIC by liver biopsy or by an FDA-cleared or approved method for identifying patients for treatment with deferasirox therapy Serum ferritin level on at least 2 measurements 1 month apart [see Clinical Studies (14)] Baseline serum creatinine in duplicate (due to variations in measurements) and determine the creatinine clearance (Cockcroft-Gault method) [see Dosage and Administration (2.4), Warnings and Precautions (5.1)] Serum transaminases and bilirubin [see Dosage and Administration (2.4), Warnings and Precautions (5.2)] Baseline auditory and ophthalmic examinations [see Warnings and Precautions (5.9)]Initiating therapy:
The recommended initial dose of Exjade is 10 mg per kg body weight orally once daily. Calculate doses (mg per kg per day) to the nearest whole tablet. If the baseline LIC is greater than 15 mg Fe/g dw, consider increasing the dose to 20 mg/kg/day after 4 weeks.During therapy:
Monitor serum ferritin monthly. Interrupt treatment when serum ferritin is less than 300 mcg/L and obtain an LIC to determine whether the LIC has fallen to less than 3 mg Fe/g dw. Monitor LIC every 6 months. After 6 months of therapy, if the LIC remains greater than 7 mg Fe/g dw, increase the dose of deferasirox to a maximum of 20 mg/kg/day. Do not exceed a maximum of 20 mg/kg/day. If after 6 months of therapy, the LIC is 3-7 mg Fe/g dw, continue treatment with deferasirox at no more than 10 mg/kg/day. When the LIC is less than 3 mg Fe/g dw, interrupt treatment with deferasirox and continue to monitor the LIC. Monitor blood counts, hepatic function, and renal function [see Warnings and Precautions (5.1, 5.2, 5.4)].Restart treatment when the LIC rises again to more than 5 mg Fe/g dw.
2.3 AdministrationDo not chew tablets or swallow them whole.
Take Exjade once daily on an empty stomach at least 30 minutes before food, preferably at the same time each day. Completely disperse tablets by stirring in water, orange juice, or apple juice until a fine suspension is obtained. Disperse doses of less than 1 g in 3.5 ounces of liquid and doses of 1 g or greater in 7 ounces of liquid. After swallowing the suspension, resuspend any residue in a small volume of liquid and swallow. Do not take Exjade with aluminum-containing antacid products [see Drug Interactions (7.1)].
2.4 Use in Patients with Baseline Hepatic or Renal ImpairmentPatients with Baseline Hepatic Impairment
Mild (Child-Pugh A) hepatic impairment: No dose adjustment is necessary.
Moderate (Child-Pugh B) hepatic impairment: Reduce the starting dose by 50%.
Severe (Child-Pugh C) hepatic impairment: Avoid Exjade [see Warnings and Precautions (5.2), Use in Specific Populations (8.7)].
Patients with Baseline Renal Impairment
For patients with renal impairment (ClCr 40–60 mL/min), reduce the starting dose by 50% [see Use in Specific Populations (8.6)]. Do not use Exjade in patients with serum creatinine greater than 2 times the upper limit of normal or creatinine clearance less than 40 mL/min [see Contraindications (4)].
2.5 Dose Modifications for Increases in Serum Creatinine on ExjadeFor serum creatinine increases while receiving Exjade [see Warnings and Precautions (5.1)] modify the dose as follows:
Transfusional Iron Overload
Adults and Adolescents (ages 16 years and older):
If the serum creatinine increases by 33% or more above the average baseline measurement, repeat the serum creatinine within 1 week, and if still elevated by 33% or more, reduce the dose by 10 mg per kg.Pediatric Patients (ages 2-15 years):
Reduce the dose by 10 mg per kg if serum creatinine increases to greater than 33% above the average baseline measurement and greater than the age appropriate upper limit of normal.All Patients (regardless of age):
Discontinue therapy for serum creatinine greater than 2 times the age-appropriate upper limit of normal or for creatinine clearance <40 mL/min [see Contraindications (4)].Non-Transfusion-Dependent Thalassemia Syndromes
Adults and Adolescents (ages 16 years and older):
If the serum creatinine increases by 33% or more above the average baseline measurement, repeat the serum creatinine within 1 week, and if still elevated by 33% or more, interrupt therapy if the dose is 5 mg per kg, or reduce by 50% if the dose is 10 or 20 mg per kg.Pediatric Patients (ages 10-15 years):
Reduce the dose by 5 mg per kg if serum creatinine increases to greater than 33% above the average baseline measurement and greater than the age appropriate upper limit of normal.All Patients (regardless of age):
Discontinue therapy for serum creatinine greater than 2 times the age-appropriate upper limit of normal or for creatinine clearance <40 mL/min [see Contraindications (4)]. 2.6 Dose Modifications Based on Concomitant MedicationsUDP-glucuronosyltransferases (UGT) Inducers
Concomitant use of UGT inducers decreases Exjade systemic exposure. Avoid the concomitant use of potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir) with Exjade. If you must administer Exjade with 1 of these agents, consider increasing the initial dose of Exjade by 50%, and monitor serum ferritin levels and clinical responses for further dose modification [see Dosage and Administration (2.1, 2.2), Drug Interactions (7.5)].
Bile Acid Sequestrants
Concomitant use of bile acid sequestrants decreases Exjade systemic exposure. Avoid the concomitant use of bile acid sequestrants (e.g., cholestyramine, colesevelam, colestipol) with Exjade. If you must administer Exjade with 1 of these agents, consider increasing the initial dose of Exjade by 50%, and monitor serum ferritin levels and clinical responses for further dose modification [see Dosage and Administration (2.1, 2.2), Drug Interactions (7.6)].
Login To Your Free Account