FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Bcg Vaccine Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Administration should be by the percutaneous route with the multiple puncture device as described below. DO NOT INJECT INTRAVENOUSLY, SUBCUTANEOUSLY, INTRAMUSCULARLY, OR INTRADERMALLY.
Although BCG vaccination often results in local adverse effects, serious or long-term complications are rare. Reactions that can be expected after vaccination include moderate axillary or cervical lymphadenopathy and induration and subsequent pustule formation at the injection site; these reactions can persist for as long as 3 months after vaccination. More severe local reactions include ulceration at the vaccination site, regional suppurative lymphadenitis with draining sinuses, and caseous lesions or purulent drainage at the puncture site; these manifestations might occur within the 5 months after vaccination and could persist for several weeks.
Acute, localized irritative toxicities of BCG may be accompanied by systemic manifestations, consistent with a "flu-like" syndrome. Systemic adverse effects of 1–2 days' duration such as fever, anorexia, myalgia, and neuralgia, often reflect hypersensitivity reactions. However, symptoms such as fever of 103°F or greater, or acute localized inflammation persisting longer than 2–3 days suggest active infections, and evaluation for serious infectious complication should be considered. If a BCG infection is suspected, the physician should consult with an infectious disease expert before therapy is initiated. Treatment should be started without delay. In patients who develop persistent fever or experience an acute febrile illness consistent with BCG infection, two or more antimycobacterial agents should be administered while diagnostic evaluation, including cultures, is conducted. Negative cultures do not necessarily rule out infection. Physicians or persons caring for patients that use this product should be familiar with the literature on prevention, diagnosis, and treatment of BCG-related complications and, when appropriate, should consult an infectious disease specialist or other physician with experience in the diagnosis and treatment of mycobacterial infections.
The most serious complication of BCG vaccination is disseminated BCG infection. BCG osteitis affecting the epiphyses of the long bones, particularly the epiphyses of the leg, can occur from 4 months to 2 years after vaccination. Fatal disseminated BCG disease has occurred at a rate of 0.06–1.56 cases per million doses of vaccine administered; these deaths occurred primarily among immunocompromised persons.{3} The appropriate therapy for systemic BCG infections is discussed in the ADVERSE REACTIONS section.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
BCG VACCINE (TICE® strain) is indicated for the prevention of tuberculosis in persons not previously infected with M. tuberculosis who are at high risk for exposure. As with any vaccine, immunization with BCG VACCINE may not protect 100% of susceptible individuals.
The Advisory Committee on Immunization Practices (ACIP) and the Advisory Committee for the Elimination of Tuberculosis has recommended that BCG vaccination be considered in the following circumstances.{3}
BCG vaccination is recommended for infants and children with negative tuberculin skin tests who are (a) at high risk of intimate and prolonged exposure to persistently untreated or ineffectively treated patients with infectious pulmonary tuberculosis and who cannot be removed from the source of exposure and cannot be placed on long-term primary preventive therapy, or (b) continuously exposed to persons with infectious pulmonary tuberculosis who have bacilli resistant to isoniazid and rifampin, and the child cannot be separated from the presence of the infectious patient.{3}
BCG vaccination of HCWs should be considered on an individual basis in settings where (a) a high percentage of TB patients are infected with M. tuberculosis strains resistant to both isoniazid and rifampin, (b) transmission of such drug resistant M. tuberculosis strains to HCWs and subsequent infection are likely, and (c) comprehensive TB infection control precautions have been implemented and have not been successful. Vaccination should not be required for employment or for assignment of HCWs in specific work areas. HCWs considered for BCG vaccination should be counseled regarding the risks and benefits associated with both BCG vaccinations and TB preventive therapy.{3}
BCG vaccination is not recommended for HCWs in settings in which the risk for M. tuberculosis transmission is low.{3}
History
There is currently no drug history available for this drug.
Other Information
BCG VACCINE for percutaneous use is an attenuated, live culture preparation of the Bacillus of Calmette and Guerin (BCG) strain of Mycobacterium bovis.{1} The TICE® strain used in this BCG VACCINE preparation was developed at the University of Illinois from a strain originated at the Pasteur Institute.
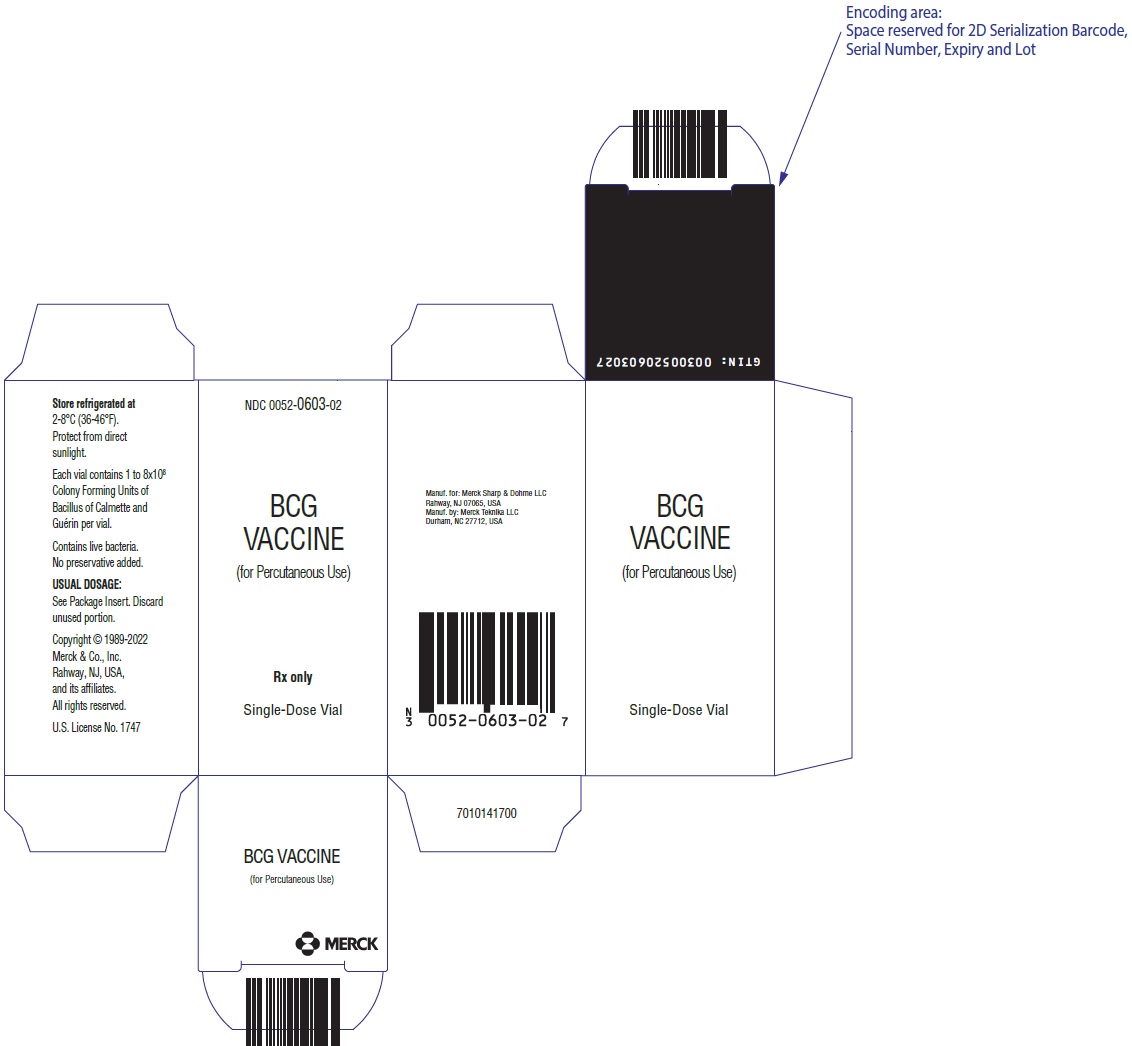
The medium in which the TICE® BCG organism is grown for preparation of the freeze-dried cake is composed of the following ingredients: glycerin, asparagine, citric acid, potassium phosphate, magnesium sulfate, and iron ammonium citrate. The final preparation prior to freeze drying also contains lactose. The freeze-dried BCG preparation is delivered in vials, each containing 1 to 8 × 108 colony forming units (CFU) of BCG which is equivalent to approximately 50 mg wet weight. Determination of in-vitro potency is achieved through colony counts derived from a serial dilution assay. Intradermal guinea pig testing is also used as an indirect measure of potency.
Reconstitution requires addition of Sterile Water for Injection, USP at 4-25°C (39-77°F). For an adult dosage, 1 mL of Sterile Water for Injection, USP, should be added to one vial of vaccine. For a pediatric dosage, 2 mL of Sterile Water for Injection, USP, should be added to one vial of vaccine (see DOSAGE AND ADMINISTRATION).
No preservatives have been added.
Sources
Bcg Vaccine Manufacturers
-
Organon Usa Inc.
![Bcg Vaccine (Bacillus Calmette-guerin Substrain Tice Live Antigen) Injection, Powder, Lyophilized, For Solution [Organon Usa Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Bcg Vaccine | Organon Usa Inc.
![Bcg Vaccine (Bacillus Calmette-guerin Substrain Tice Live Antigen) Injection, Powder, Lyophilized, For Solution [Organon Usa Inc.] Bcg Vaccine (Bacillus Calmette-guerin Substrain Tice Live Antigen) Injection, Powder, Lyophilized, For Solution [Organon Usa Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Preparation of AgentThe preparation of the BCG VACCINE suspension should be done using aseptic technique. To avoid cross-contamination, parenteral drugs should not be prepared in areas where BCG VACCINE has been prepared. A separate area for the preparation of the BCG VACCINE suspension is recommended. All equipment, supplies and receptacles in contact with BCG VACCINE should be handled and disposed of as biohazardous. The pharmacist or individual responsible for mixing the agent should wear gloves, and take precautions to avoid contact of BCG with broken skin. If preparation cannot be performed in a biocontainment hood, then a mask and gown should be worn to avoid inhalation of BCG organisms and inadvertent exposure to broken skin.
Using aseptic methods, 1 mL of Sterile Water for Injection, USP at 4-25°C (39-77°F), is added to one vial of vaccine (see Pediatric Dose below for pediatric use). Gently swirl the vial until a homogenous suspension is obtained. Avoid forceful agitation which may cause clumping of the mycobacteria.
Persons administering vaccines should take necessary precautions to minimize risk for spreading disease. Hands should be washed before each new patient is seen. Syringes and needles used for applications must be sterile and preferably disposable to minimize the risk of contamination. A separate needle and syringe should be used for each application. Disposable needles and the multiple puncture device should be discarded as biohazardous waste in labeled, puncture-proof containers to prevent inadvertent needlestick injury or reuse.{22} After use, any unused vaccine and all materials exposed to the product should be immediately placed in a biohazard container and disposed of in an appropriate manner.
Reconstituted vaccine should be kept refrigerated, protected from exposure to direct sunlight, and used within 2 hours. Freezing of the reconstituted product is not recommended.
Note: DO NOT filter the contents of the BCG VACCINE vial. Precautions should be taken to avoid exposing the BCG VACCINE to direct sunlight. Bacteriostatic solutions must be avoided. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Reconstitution should result in a uniform suspension of the bacilli.
Treatment and ScheduleBCG vaccination is reserved for persons who have a reaction of less than 5mm induration after skin testing with 5 TU of PPD tuberculin. The preferred method of skin testing is the Mantoux tuberculin skin-test using 0.1 mL of 5 tuberculin units (TU) of PPD.{3} It is recommended that a Mantoux skin-test be performed prior to BCG vaccination to demonstrate the absence of tuberculous infection.
The vaccine is to be administered after fully explaining the risks and benefits to the vaccinee, parent, or guardian. BCG vaccination should not be given to individuals previously infected with M. tuberculosis. The vaccine is administered percutaneously utilizing a sterile multiple puncture device. The multiple puncture device consists of a plastic holder for a thin, wafer-like stainless steel plate 7/8" by 1 1/8", from which 36 points protrude. After the vaccine is prepared, the skin site is cleansed with an alcohol or acetone sponge and allowed to dry thoroughly.
1. Administer the vaccine in the deltoid region (Figure 1). Position the arm to maintain a horizontal surface where the vaccine is to be placed.Figure 1
2. Drop the immunizing dose of 0.2–0.3 mL of BCG VACCINE from the syringe and needle onto the cleansed surface of the skin (Figure 2) and spread over a 1" by 2" area using the edge of the multiple puncture device (Figure 3).Figure 2
Figure 3
3. Grasp the arm firmly from underneath, tensing the skin. Center the multiple puncture device over the vaccine and apply firm downward pressure such that the device points are well buried in the skin (Figure 4).Figure 4
4. Maintain pressure for 5 seconds. Do not "rock" the device. Release the pressure underneath the arm and remove the device. In a successful procedure the points puncture the skin. If the points do not puncture the skin, the procedure must be repeated. 5. After successful puncture, spread vaccine as evenly as possible over the puncture area with the edge of the device. An additional 1–2 drops of BCG VACCINE may be added to ensure a very wet vaccination site. 6. Use the multiple puncture device once and discard in a standard biohazardous sharps container. 7. Loosely cover the site and keep dry for 24 hours. 8. Advise the patient that the vaccine contains live organisms. Although the vaccine will not survive in a dry state for long, infection of others is possible.Tuberculin reactivity resulting from BCG vaccination should be documented. A vaccinated person should be tuberculin skin tested 2–3 months after BCG administration, and the test results, in millimeters of induration, should be recorded in the person's medical record.{9} Vaccination should be repeated for those who remain tuberculin negative to 5 TU of tuberculin after 2–3 months.
Pediatric DoseDo not administer INTRAVENOUSLY, SUBCUTANEOUSLY, INTRAMUSCULARLY, OR INTRADERMALLY. Administer the vaccine in the deltoid region.
In infants less than 1 month old, the dosage of BCG VACCINE should be reduced by one-half, by using 2 mL of Sterile Water for Injection, USP at 4-25°C (39-77°F) when reconstituting. If a vaccinated infant remains tuberculin negative to 5 TU on skin testing, and if indications for vaccination persist, the infant should receive a full dose after 1 year of age.
Login To Your Free Account