FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Gabapentin Solution Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Antiepileptic drugs (AEDs), including gabapentin oral solution, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events Per 1000 Patients | Drug Patients with Events Per 1000 Patients | Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients | Risk Difference: Additional Drug Patients with Events Per 1000 Patients |
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing gabapentin oral solution or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Gabapentin use in pediatric patients with epilepsy 3-12 years of age is associated with the occurrence of central nervous system related adverse events. The most significant of these can be classified into the following categories: 1) emotional lability (primarily behavioral problems), 2) hostility, including aggressive behaviors, 3) thought disorder, including concentration problems and change in school performance, and 4) hyperkinesia (primarily restlessness and hyperactivity). Among the gabapentin-treated patients, most of the events were mild to moderate in intensity.
In controlled trials in pediatric patients 3-12 years of age the incidence of these adverse events was: emotional lability 6% (gabapentin-treated patients) vs 1.3% (placebo-treated patients); hostility 5.2% vs 1.3%; hyperkinesia 4.7% vs 2.9%; and thought disorder 1.7% vs 0%. One of these events, a report of hostility, was considered serious. Discontinuation of gabapentin treatment occurred in 1.3% of patients reporting emotional lability and hyperkinesia and 0.9% of gabapentin-treated patients reporting hostility and thought disorder. One placebo-treated patient (0.4%) withdrew due to emotional lability.
Antiepileptic drugs should not be abruptly discontinued because of the possibility of increasing seizure frequency.
In the placebo-controlled studies in patients >12 years of age the incidence of status epilepticus in patients receiving gabapentin was 0.6% (3 of 543) versus 0.5% in patients receiving placebo (2 of 378). Among the 2074 patients >12 years of age treated with gabapentin across all studies (controlled and uncontrolled) 31 (1.5%) had status epilepticus. Of these, 14 patients had no prior history of status epilepticus either before treatment or while on other medications. Because adequate historical data are not available, it is impossible to say whether or not treatment with gabapentin is associated with a higher or lower rate of status epilepticus than would be expected to occur in a similar population not treated with gabapentin.
In standard preclinical in vivo lifetime carcinogenicity studies, an unexpectedly high incidence of pancreatic acinar adenocarcinomas was identified in male, but not female, rats. (See PRECAUTIONS: Carcinogenesis, Mutagenesis, Impairment of Fertility.) The clinical significance of this finding is unknown. Clinical experience during gabapentin's premarketing development provides no direct means to assess its potential for inducing tumors in humans.
In clinical studies in adjunctive therapy in epilepsy comprising 2085 patient-years of exposure in patients >12 years of age, new tumors were reported in 10 patients (2 breast, 3 brain, 2 lung, 1 adrenal, 1 non-Hodgkin's lymphoma, 1 endometrial carcinoma in situ), and preexisting tumors worsened in 11 patients (9 brain, 1 breast, 1 prostate) during or up to 2 years following discontinuation of gabapentin. Without knowledge of the background incidence and recurrence in a similar population not treated with gabapentin, it is impossible to know whether the incidence seen in this cohort is or is not affected by treatment.
During the course of premarketing development of gabapentin 8 sudden and unexplained deaths were recorded among a cohort of 2203 patients treated (2103 patient-years of exposure).
Some of these could represent seizure-related deaths in which the seizure was not observed, e.g., at night. This represents an incidence of 0.0038 deaths per patient-year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving gabapentin (ranging from 0.0005 for the general population of epileptics to 0.003 for a clinical trial population similar to that in the gabapentin program, to 0.005 for patients with refractory epilepsy). Consequently, whether these figures are reassuring or raise further concern depends on comparability of the populations reported upon to the gabapentin cohort and the accuracy of the estimates provided.
Drug Reaction with Eosinophilia and Systemetic Symptoms (DRESS), also known as multiorgan hypersensitivity, has been reported in patients taking antiepileptic drugs, including Gabapentin. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, and/or lymphadenopathy, in association with other organ system involvement, such as hepatitis, nephritis, hematological abnormalities, myocarditis or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its expression, other organ systems not noted may be involved.
It is important to note that the early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. Gabapentin Oral Solution should be discontinued if an alternative etiology for the signs or symptoms cannot be established.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Gabapentin oral solution is indicated for the management of postherpetic neuralgia in adults.
Gabapentin oral solution is indicated as adjunctive therapy in the treatment of partial seizures with and without secondary generalization in patients over 12 years of age with epilepsy. Gabapentin oral solution is also indicated as adjunctive therapy in the treatment of partial seizures in pediatric patients age 3 - 12 years.
History
There is currently no drug history available for this drug.
Other Information
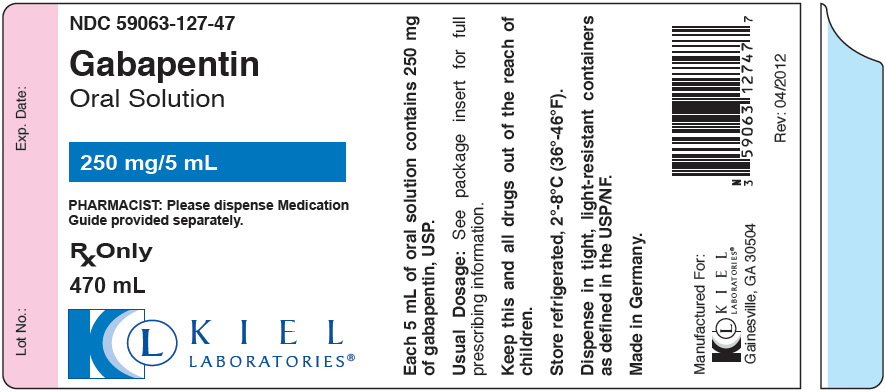
Gabapentin oral solution is supplied as an oral solution containing 250 mg/5 mL of gabapentin. The inactive ingredients for the oral solution are anise flavor, artificial strawberry flavor, glycerin, hydrochloric acid, purified water, sodium hydroxide and xylitol.
Gabapentin is described as 1-(aminomethyl) cyclohexaneacetic acid with a molecular formula of C9H17NO2 and a molecular weight of 171.24. The structural formula of gabapentin is:

Gabapentin is a white to off-white crystalline solid with a pKa1 of 3.7 and a pKa2 of 10.7. It is freely soluble in water and both basic and acidic aqueous solutions. The log of the partition coefficient (n-octanol/0.05M phosphate buffer) at pH 7.4 is -1.25.
Sources
Gabapentin Solution Manufacturers
-
Kiel Laboratories, Inc.
![Gabapentin Solution [Kiel Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Solution | Kiel Laboratories, Inc.
![Gabapentin Solution [Kiel Laboratories, Inc.] Gabapentin Solution [Kiel Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin oral solution is given orally with or without food.
If gabapentin oral solution is reduced, discontinued or substituted with an alternative medication, this should be done gradually over a minimum of 1 week (a longer period may be needed at the discretion of the prescriber).
Postherpetic NeuralgiaIn adults with postherpetic neuralgia, gabapentin therapy may be initiated as a single 300-mg dose on Day 1, 600 mg/day on Day 2 (divided BID), and 900 mg/day on Day 3 (divided TID). The dose can subsequently be titrated up as needed for pain relief to a daily dose of 1800 mg (divided TID). In clinical studies, efficacy was demonstrated over a range of doses from 1800 mg/day to 3600 mg/day with comparable effects across the dose range. Additional benefit of using doses greater than 1800 mg/day was not demonstrated.
EpilepsyGabapentin oral solution is recommended for add-on therapy in patients 3 years of age and older. Effectiveness in pediatric patients below the age of 3 years has not been established.
Patients >12 years of age: The effective dose of gabapentin is 900 to 1800 mg/day and given in divided doses (three times a day). The starting dose is 300 mg three times a day. If necessary, the dose may be increased three times a day up to 1800 mg/day. Dosages up to 2400 mg/day have been well tolerated in long-term clinical studies. Doses of 3600 mg/day have also been administered to a small number of patients for a relatively short duration, and have been well tolerated. The maximum time between doses in the TID schedule should not exceed 12 hours.
Pediatric Patients Age 3-12 years: The starting dose should range from 10-15 mg/kg/day in 3 divided doses, and the effective dose reached by upward titration over a period of approximately 3 days. The effective dose of gabapentin in patients 5 years of age and older is 25-35 mg/kg/day and given in divided doses (three times a day). The effective dose in pediatric patients ages 3 and 4 years is 40 mg/kg/day and given in divided doses (three times a day) (see CLINICAL PHARMACOLOGY, Pediatrics.) Dosages up to 50 mg/kg/day have been well-tolerated in a long-term clinical study. The maximum time interval between doses should not exceed 12 hours.
It is not necessary to monitor gabapentin plasma concentrations to optimize gabapentin therapy. Further, because there are no significant pharmacokinetic interactions among gabapentin and other commonly used antiepileptic drugs, the addition of gabapentin does not alter the plasma levels of these drugs appreciably.
If gabapentin oral solution is discontinued and/or an alternate anticonvulsant medication is added to the therapy, this should be done gradually over a minimum of 1 week.
Dosage in Renal ImpairmentCreatinine clearance is difficult to measure in outpatients. In patients with stable renal function, creatinine clearance (CCr) can be reasonably well estimated using the equation of Cockcroft and Gault:
for females CCr=(0.85)(140-age)(weight)/[(72)(SCr)]
for males CCr=(140-age)(weight)/[(72)(SCr)]where age is in years, weight is in kilograms and SCr is serum creatinine in mg/dL.
Dosage adjustment in patients ≥12 years of age with compromised renal function or undergoing hemodialysis is recommended as follows (see dosing recommendations above for effective doses in each indication).
TABLE 6. Gabapentin Dosage Based on Renal Function a For patients with creatinine clearance <15 mL/min, reduce daily dose in proportion to creatinine clearance (e.g. patients with a creatinine clearance of 7.5 mL/min should receive one-half the daily dose that patients with a creatinine clearance of 15 mL/min receive).
b Patients on hemodialysis should receive maintenance doses based on estimates of creatinine clearance as indicated in the upper portion of the table and a supplemental post-hemodialysis dose administered after each 4 hours of hemodialysis as indicated in the lower portion of the table. Renal Function
Creatinine Clearance
(mL/min) Total Daily
Dose Range
(mg/day) Dose Regimen
(mg) ≥60 900 - 3600 300 TID 400 TID 600 TID 800 TID 1200 TID >30 - 59 400 - 1400 200 BID 300 BID 400 BID 500 BID 700 BID >15 - 29 200 - 700 200 QD 300 QD 400 QD 500 QD 700 QD 15a 100 - 300 100 QD 125 QD 150 QD 200 QD 300 QD
Post-Hemodialysis Supplemental Dose (mg)b
Hemodialysis 125b 150b 200b 250b 350bThe use of gabapentin in patients <12 years of age with compromised renal function has not been studied.
Dosage in ElderlyBecause elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients.
-
Acella Pharmaceuticals, Llc
![Gabapentin Solution [Acella Pharmaceuticals, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Solution | Acella Pharmaceuticals, Llc
![Gabapentin Solution [Acella Pharmaceuticals, Llc] Gabapentin Solution [Acella Pharmaceuticals, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Oral Solution is given orally with or without food.
If Gabapentin Oral Solution is reduced, discontinued or substituted with an alternative medication, this should be done gradually over a minimum of 1 week (a longer period may be needed at the discretion of the prescriber).
Postherpetic NeuralgiaIn adults with postherpetic neuralgia, gabapentin therapy may be initiated as a single 300-mg dose on Day 1, 600 mg/day on Day 2 (divided BID), and 900 mg/day on Day 3 (divided TID). The dose can subsequently be titrated up as needed for pain relief to a daily dose of 1800 mg (divided TID). In clinical studies, efficacy was demonstrated over a range of doses from 1800 mg/day to 3600 mg/day with comparable effects across the dose range. Additional benefit of using doses greater than 1800 mg/day was not demonstrated.
EpilepsyGabapentin Oral Solution is recommended for add-on therapy in patients 3 years of age and older. Effectiveness in pediatric patients below the age of 3 years has not been established.
Patients >12 years of age: The effective dose of Gabapentin Oral Solution is 900 to 1800 mg/day and given in divided doses (three times a day). The starting dose is 300 mg three times a day. If necessary, the dose may be increased three times a day up to 1800 mg/day. Dosages up to 2400 mg/day have been well tolerated in long-term clinical studies. Doses of 3600 mg/day have also been administered to a small number of patients for a relatively short duration, and have been well tolerated. The maximum time between doses in the TID schedule should not exceed 12 hours.
Pediatric Patients Age 3-12 years: The starting dose should range from 10-15 mg/kg/day in 3 divided doses, and the effective dose reached by upward titration over a period of approximately 3 days. The effective dose of gabapentin in patients 5 years of age and older is 25-35 mg/kg/day and given in divided doses (three times a day). The effective dose in pediatric patients ages 3 and 4 years is 40 mg/kg/day and given in divided doses (three times a day). (See CLINICAL PHARMACOLOGY, Pediatrics.) Dosages up to 50 mg/kg/day have been well-tolerated in a long-term clinical study. The maximum time interval between doses should not exceed 12 hours.
It is not necessary to monitor gabapentin plasma concentrations to optimize gabapentin therapy. Further, because there are no significant pharmacokinetic interactions among gabapentin and other commonly used antiepileptic drugs, the addition of gabapentin does not alter the plasma levels of these drugs appreciably.
If Gabapentin Oral Solution is discontinued and/or an alternate anticonvulsant medication is added to the therapy, this should be done gradually over a minimum of 1 week.
Dosage in Renal ImpairmentCreatinine clearance is difficult to measure in outpatients. In patients with stable renal function, creatinine clearance (CCr) can be reasonably well estimated using the equation of Cockcroft and Gault:
for females CCr=(0.85)(140-age)(weight)/[(72)(SCr)]
for males CCr=(140-age)(weight)/[(72)(SCr)]where age is in years, weight is in kilograms and SCr is serum creatinine in mg/dL.
Dosage adjustment in patients ≥12 years of age with compromised renal function or undergoing hemodialysis is recommended as follows (see dosing recommendations above for effective doses in each indication).
TABLE 6. Gabapentin Dosage Based on Renal Function * For patients with creatinine clearance <15 mL/min, reduce daily dose in proportion to creatinine clearance (e.g. patients with a creatinine clearance of 7.5 mL/min should receive one-half the daily dose that patients with a creatinine clearance of 15 mL/min receive). † Patients on hemodialysis should receive maintenance doses based on estimates of creatinine clearance as indicated in the upper portion of the table and a supplemental post-hemodialysis dose administered after each 4 hours of hemodialysis as indicated in the lower portion of the table. Renal Function
Creatinine Clearance
(mL/min) Total Daily
Dose Range
(mg/day) Dose Regimen
(mg) ≥60 900 - 3600 300 TID 400 TID 600 TID 800 TID 1200 TID >30 - 59 400 - 1400 200 BID 300 BID 400 BID 500 BID 700 BID >15 - 29 200 - 700 200 QD 300 QD 400 QD 500 QD 700 QD 15* 100 - 300 100 QD 125 QD 150 QD 200 QD 300 QD
Post-Hemodialysis Supplemental Dose (mg)† Hemodialysis 125† 150† 200† 250† 350†The use of gabapentin in patients <12 years of age with compromised renal function has not been studied.
Dosage in ElderlyBecause elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients.
-
Hi-tech Pharmacal Co., Inc.
![Gabapentin Solution [Hi-tech Pharmacal Co., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Solution | Pd-rx Pharmaceuticals, Inc.
![Gabapentin Solution [Hi-tech Pharmacal Co., Inc.] Gabapentin Solution [Hi-tech Pharmacal Co., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosage must be adjusted to individual patient needs.
2.1 Oral Dosage and Administration in AdultsThe recommended initial dose is 20 mg four times a day.
After one week treatment with the initial dose, the dose may be increased to 40 mg four times a day unless side effects limit dosage escalation.
If efficacy is not achieved within 2 weeks or side effects require doses below 80 mg per day, the drug should be discontinued. Documented safety data are not available for doses above 80 mg daily for periods longer than 2 weeks.
-
Taro Pharmaceuticals U.s.a., Inc.
![Gabapentin Solution [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Solution | Taro Pharmaceuticals U.s.a., Inc.
![Gabapentin Solution [Taro Pharmaceuticals U.s.a., Inc.] Gabapentin Solution [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin is given orally with or without food.
If gabapentin dose is reduced, discontinued, or substituted with an alternative medication, this should be done gradually over a minimum of 1 week (a longer period may be needed at the discretion of the prescriber).
Postherpetic NeuralgiaIn adults with postherpetic neuralgia, gabapentin therapy may be initiated as a single 300-mg dose on Day 1, 600 mg/day on Day 2 (divided BID), and 900 mg/day on Day 3 (divided TID). The dose can subsequently be titrated up as needed for pain relief to a daily dose of 1800 mg (divided TID). In clinical studies, efficacy was demonstrated over a range of doses from 1800 mg/day to 3600 mg/day with comparable effects across the dose range. Additional benefit of using doses greater than 1800 mg/day was not demonstrated.
EpilepsyGabapentin is recommended for add-on therapy in patients 3 years of age and older. Effectiveness in pediatric patients below the age of 3 years has not been established.
Patients >12 years of ageThe effective dose of gabapentin is 900 to 1800 mg/day and given in divided doses (three times a day) using 300 or 400 mg capsules. The starting dose is 300 mg three times a day. If necessary, the dose may be increased using 300 or 400 mg capsules three times a day up to 1800 mg/day. Dosages up to 2400 mg/day have been well tolerated in long-term clinical studies. Doses of 3600 mg/day have also been administered to a small number of patients for a relatively short duration, and have been well tolerated. The maximum time between doses in the TID schedule should not exceed 12 hours.
Pediatric Patients Age 3 to 12 yearsThe starting dose should range from 10 to 15 mg/kg/day in 3 divided doses, and the effective dose reached by upward titration over a period of approximately 3 days. The effective dose of gabapentin in patients 5 years of age and older is 25 to 35 mg/kg/day and given in divided doses (three times a day). The effective dose in pediatric patients ages 3 and 4 years is 40 mg/kg/day and given in divided doses (three times a day) (see CLINICAL PHARMACOLOGY, Pediatric). Dosages up to 50 mg/kg/day have been well tolerated in a long-term clinical study. The maximum time interval between doses should not exceed 12 hours.
It is not necessary to monitor gabapentin plasma concentrations to optimize gabapentin therapy. Further, because there are no significant pharmacokinetic interactions among gabapentin and other commonly used antiepileptic drugs, the addition of gabapentin does not alter the plasma levels of these drugs appreciably.
If gabapentin is discontinued and/or an alternate anticonvulsant medication is added to the therapy, this should be done gradually over a minimum of 1 week.
Dosage in Renal ImpairmentCreatinine clearance is difficult to measure in outpatients. In patients with stable renal function, creatinine clearance (CCr) can be reasonably well estimated using the equation of Cockcroft and Gault:
for females C Cr = (0.85)(140-age)(weight)/[(72)(S Cr)] for males C Cr = (140-age)(weight)/[(72)(S Cr)]in which age is in years, weight is in kilograms, and SCr is serum creatinine in mg/dL.
Dosage adjustment in patients ≥ 12 years of age with compromised renal function or undergoing hemodialysis is recommended as follows (see dosing recommendations above for effective doses in each indication).
TABLE 6. Gabapentin Dosage Based on Renal Function Renal Function Creatinine Clearance (mL/min) Total Daily Dose Range (mg/day) Dose Regimen (mg) * For patients with creatinine clearance <15 mL/min, reduce daily dose in proportion to creatinine clearance (e.g., patients with a creatinine clearance of 7.5 mL/min should receive one-half the daily dose that patients with a creatinine clearance of 15 mL/min receive). † Patients on hemodialysis should receive maintenance doses based on estimates of creatinine clearance as indicated in the upper portion of the table and a supplemental post-hemodialysis dose administered after each 4 hours of hemodialysis as indicated in the lower portion of the table. ≥60 900 to 3600 300 TID 400 TID 600 TID 800 TID 1200 TID >30 to 59 400 to 1400 200 BID 300 BID 400 BID 500 BID 700 BID >15 to 29 200 to 700 200 QD 300 QD 400 QD 500 QD 700 QD 15* 100 to 300 100 QD 125 QD 150 QD 200 QD 300 QD Post-Hemodialysis Supplemental Dose (mg)† Hemodialysis 125† 150† 200† 250† 350†The use of gabapentin in patients <12 years of age with compromised renal function has not been studied.
Dosage in ElderlyBecause elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients.
-
Amneal Pharmaceuticals Of New York, Llc
![Gabapentin Solution [Amneal Pharmaceuticals Of New York, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Gabapentin Solution | Amneal Pharmaceuticals Of New York, Llc
![Gabapentin Solution [Amneal Pharmaceuticals Of New York, Llc] Gabapentin Solution [Amneal Pharmaceuticals Of New York, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
The dose, concentration, and infusion rate of intravenous fosphenytoin should always be expressed as phenytoin sodium equivalents (PE). There is no need to perform molecular weight-based adjustments when converting between fosphenytoin and phenytoin sodium doses. Fosphenytoin should always be prescribed and dispensed in phenytoin sodium equivalent units (PE). 1.5 mg of fosphenytoin sodium is equivalent to 1 mg phenytoin sodium, and is referred to as 1 mg PE. The amount and concentration of fosphenytoin is always expressed in terms of mg of phenytoin sodium equivalents (mg PE).
Do not confuse the concentration of fosphenytoin with the total amount of drug in the vial.
Caution must be used when administering fosphenytoin due to the risk of dosing errors (see WARNINGS). Medication errors associated with fosphenytoin have resulted in patients receiving the wrong dose of fosphenytoin. Fosphenytoin is marketed in 2 mL vials containing a total of 100 mg PE and 10 mL vials containing a total of 500 mg PE. Both vials contain a concentration of 50 mg PE/mL. Errors have occurred when the concentration of the vial (50 mg PE/mL) was misinterpreted to mean that the total content of the vial was 50 mg PE. These errors have resulted in two- or ten-fold overdoses of fosphenytoin since each of the vials actually contains a total of 100 mg PE or 500 mg PE. In some cases, ten-fold overdoses were associated with fatal outcomes. To help minimize confusion, the prescribed dose of fosphenytoin should always be expressed in milligrams of phenytoin equivalents (mg PE). Additionally, when ordering and storing fosphenytoin, consider displaying the total drug content (i.e., 100 mg PE/ 2 mL or 500 mg PE/ 10 mL) instead of concentration in computer systems, pre-printed orders, and automated dispensing cabinet databases to help ensure that total drug content can be clearly identified. Care should be taken to ensure the appropriate volume of fosphenytoin is withdrawn from the vial when preparing the dose for administration. Attention to these details may prevent some fosphenytoin medication errors from occurring.
Prior to intravenous infusion, dilute fosphenytoin injection in 5% dextrose or 0.9% saline solution for injection to a concentration ranging from 1.5 to 25 mg PE/mL. The maximum concentration of fosphenytoin in any solution should be 25 mg PE/mL. When fosphenytoin is given as an intravenous infusion, fosphenytoin needs to be diluted and should only be administered at a rate not exceeding 150 mg PE/min.
Parenteral drug products should be inspected visually for particulate matter or discoloration prior to administration, whenever solution and container permit.
Status Epilepticus
The loading dose of fosphenytoin is 15 to 20 mg PE/kg administered at 100 to 150 mg PE/min. Because of the risk of hypotension, fosphenytoin should be administered no faster than 150 mg PE/min. Continuous monitoring of the electrocardiogram, blood pressure, and respiratory function is essential and the patient should be observed throughout the period where maximal serum phenytoin concentrations occur, approximately 10 to 20 minutes after the end of fosphenytoin infusions. Because the full antiepileptic effect of phenytoin, whether given as fosphenytoin or parenteral phenytoin, is not immediate, other measures, including concomitant administration of an intravenous benzodiazepine, will usually be necessary for the control of status epilepticus. The loading dose should be followed by maintenance doses of either fosphenytoin or phenytoin.If administration of fosphenytoin does not terminate seizures, the use of other anticonvulsants and other appropriate measures should be considered.
Even though loading doses of fosphenytoin have been given by the intramuscular route for other indications when intravenous access is impossible, intramuscular fosphenytoin should ordinarily not be used in the treatment of status epilepticus because therapeutic phenytoin concentrations may not be reached as quickly as with intravenous administration.
Nonemergent Loading and Maintenance Dosing
Because of the risks of cardiac and local toxicity associated with intravenous fosphenytoin, oral phenytoin should be used whenever possible.
The loading dose of fosphenytoin is 10 to 20 mg PE/kg given intravenous or intramuscular. The rate of administration for intravenous fosphenytoin should be no greater than 150 mg PE/min. Continuous monitoring of the electrocardiogram, blood pressure, and respiratory function is essential and the patient should be observed throughout the period where maximal serum phenytoin concentrations occur (approximately 20 minutes after the end of fosphenytoin infusion).
The initial daily maintenance dose of fosphenytoin is 4 to 6 mg PE/kg/day in divided doses.
Intramuscular or Intravenous Substitution for Oral Phenytoin Therapy
When treatment with oral phenytoin is not possible, fosphenytoin can be substituted for oral phenytoin at the same total daily dose.
Phenytoin sodium capsules are approximately 90% bioavailable by the oral route. Phenytoin, supplied as fosphenytoin, is 100% bioavailable by both the intramuscular and intravenous routes. For this reason, plasma phenytoin concentrations may increase modestly when intramuscular or intravenous fosphenytoin is substituted for oral phenytoin sodium therapy.
The rate of administration for intravenous fosphenytoin should be no greater than 150 mg PE/min.
In controlled trials, intramuscular fosphenytoin was administered as a single daily dose utilizing either 1 or 2 injection sites. Some patients may require more frequent dosing.
Dosing in Special PopulationsPatients with Renal or Hepatic Disease: Due to an increased fraction of unbound phenytoin in patients with renal or hepatic disease, or in those with hypoalbuminemia, the interpretation of total phenytoin plasma concentrations should be made with caution (see CLINICAL PHARMACOLOGY, Special Populations). Unbound phenytoin concentrations may be more useful in these patient populations. After intravenous fosphenytoin administration to patients with renal and/or hepatic disease, or in those with hypoalbuminemia, fosphenytoin clearance to phenytoin may be increased without a similar increase in phenytoin clearance. This has the potential to increase the frequency and severity of adverse events (see PRECAUTIONS).
Elderly Patients: Age does not have a significant impact on the pharmacokinetics of fosphenytoin following fosphenytoin administration. Phenytoin clearance is decreased slightly in elderly patients and lower or less frequent dosing may be required.
Pediatric: The safety and efficacy of fosphenytoin in pediatric patients have not been established.
Login To Your Free Account


![Gabapentin Solution [Acella Pharmaceuticals, Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3255245c-6ae6-46ab-a1c1-0b8d4d4cdaa2&name=3255245c-6ae6-46ab-a1c1-0b8d4d4cdaa2-06.jpg)
![Gabapentin Solution [Hi-tech Pharmacal Co., Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=da0e1f63-cb90-4c2a-908f-7d81e672be10&name=43063045.jpg)
![Gabapentin Solution [Taro Pharmaceuticals U.s.a., Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=06b796b6-a8a7-414f-8e53-bfb17f8e5700&name=gabapentin-06.jpg)
![Gabapentin Solution [Amneal Pharmaceuticals Of New York, Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=87ff8a91-5b37-401c-b75c-dc6efd348761&name=fosphenytoin-sodium-injection-usp-3.jpg)