FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Lisinopril With Hydrochlorothiazide Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including lisinopril and hydrochlorothiazide) may be subject to a variety of adverse reactions, some of them serious.
Angioedema: Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported rarely in patients treated with angiotensin converting enzyme inhibitors, including lisinopril. This may occur at any time during treatment. In such cases lisinopril and hydrochlorothiazide should be promptly discontinued and appropriate therapy and monitoring should be provided until complete and sustained resolution of signs and symptoms has occurred. In instances where swelling has been confined to the face and lips the condition has generally resolved without treatment, although antihistamines have be useful in relieving symptoms. Angioedema associated with laryngeal edema may be fatal. Where there involvement of the tongue, glottis or Iarynx, likely to cause airway obstruction, subcutaneous epinephrine solution 1:1000 (0.3 mL to 0.5 mL) and/or measures necessary to ensure a patent airway, should be promptly provided. (See ADVERSE REACTIONS.)
Patients with a history of angioedema unrelated to ACE inhibitor therapy may at increased risk of angioedema while receiving an ACE inhibitor (see also INDICATIONS AND USAGE and CONTRAINDICATIONS).
Anaphylactoid reactions during desensitization: Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid reactions during membrane exposure: Anaphylactoid reactions have been reported in patients dialyzed with high-flux membranes and treated concomitantly with an ACE inhibitor. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
Hypotension and Related Effects: Excessive hypotension was rarely seen in uncomplicated hypertensive patients but is a possible consequence of lisinopril use in salt/volume-depleted persons, such as those treated vigorously with diuretics or patients on dialysis. (See PRECAUTIONS, Drug Interactions and ADVERSE REACTIONS.)
Syncope has been reported in 0.8 percent of patients receiving lisinopril and hydrochlorothiazide. In patients with hypertension receiving lisinopril alone, the incidence of syncope was 0.1 percent. The overall incidence of syncope may be reduced by proper titration of the individual components. (See PRECAUTIONS, Drug Interactions,ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION.)
In patients with severe congestive heart failure, with or without associated renal insufficiency, excessive hypotension has been observed and may be associated with oliguria and/or progressive azotemia, and rarely with acute renal failure and/or death. Because of the potential fall in blood pressure in these patients, therapy should be started under very close medical supervision. Such patients should be followed closely for the first two weeks of treatment and whenever the dose of lisinopril and/or diuretic is increased. Similar considerations apply to patients with ischemic heart or cerebrovascular disease in whom an excessive fall in blood pressure could result in a myocardial infarction or cerebrovascular accident.
If hypotension occurs, the patient should be placed in supine position and, if necessary, receive an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further doses which usually can be given without difficulty once the blood pressure has increased after volume expansion.
Another angiotensin converting enzyme inhibitor, captopril, has been shown to cause agranulocytosis and bone marrow depression, rarely in uncomplicated patients but more frequently in patients with renal impairment, especially if they also have a collagen vascular disease. Available data from clinical trials of lisinopril are insufficient to show that lisinopril does not cause agranulocytosis at similar rates. Marketing experience has revealed rare cases of neutropenia and bone marrow depression in which a causal relationship to lisinopril cannot be excluded. Periodic monitoring of white blood cell counts in patients with collagen vascular disease and renal disease should be considered.
Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis, and (sometimes) death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
Thiazides should be used with caution in severe renal disease. In patients with renal disease, thiazides may precipitate azotemia. Cumulative effects of the drug may develop in patients with impaired renal function.
Thiazides should be used with caution in patients with impaired hepatic function or progressive liver disease, since minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
Sensitivity reactions may occur in patients with or without a history of allergy or bronchial asthma.
The possibility of exacerbation or activation of systemic lupus erythematosus has been reported.
Lithium generally should not be given with thiazides (see PRECAUTIONS, Drug Interactions, Lisinopril and Hydrochlorothiazide).
Teratogenicity studies were conducted in mice and rats with up to 90 mg/kg/day of lisinopril in combination with 10 mg/kg/day of hydrochlorothiazide. This dose of lisinopril is 5 times (in mice) and 10 times (in rats) the maximum recommended human daily dose (MRHDD) when compared on a body surface area basis (mg/m2); the dose of hydrochlorothiazide is 0.9 times (in mice) and 1.8 times (in rats) the MRHDD. Maternal or fetotoxic effects were not seen in mice with the combination. In rats decreased maternal weight gain and decreased fetal weight occurred down to 3/10 mg/kg/day (the lowest dose tested). Associated with the decreased fetal weight was a delay in fetal ossification. The decreased fetal weight and delay in fetal ossification were not seen in saline-supplemented animals given 90/10 mg/kg/day.
When used in pregnancy during the second and third trimesters, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, lisinopril and hydrochlorothiazide should be discontinued as soon as possible. (See Lisinopril, Fetal/Neonatal Morbidity and Mortality, below.)
Fetal/Neonatal Morbidity and Mortality: ACE inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, ACE inhibitors should be discontinued as soon as possible.
The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to the ACE-inhibitor exposure.
These adverse effects do not appear to have resulted from intrauterine ACE-inhibitor exposure that has been limited to the first trimester. Mothers whose embryos and fetuses are exposed to ACE inhibitors only during the first trimester should be so informed. Nonetheless, when patients become pregnant; physicians should make every effort to discontinue the use of lisinopril and hydrochlorothiazide as soon as possible.
Rarely (probably less often than once in every thousand pregnancies), no alternative to ACE inhibitors will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses, and serial ultrasound examinations should be performed to assess the intraamniotic environment.
If oligohydramnios is observed, lisinopril and hydrochlorothiazide should be discontinued unless it is considered lifesaving for the mother. Contraction stress testing (CST), a non-stress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to ACE inhibitors should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function. Lisinopril, which crosses the placenta, has been removed from neonatal circulation by peritoneal dialysis with some clinical benefit, and theoretically may be removed by exchange transfusion, although there is no experience with the latter procedure.
No teratogenic effects of lisinopril were seen in studies of pregnant mice, rats, and rabbits. On a body surface area basis, the doses used were up 55 times, 33 times, and 0.15 times, respectively, the MRHDD.
Studies in which hydrochlorothiazide was orally administered to pregnant mice and rats during their respective periods of major organogenesis at doses up to 3000 and 1000 mg/kg/day, respectively, provided no evidence of harm to the fetus. These doses are more than 150 times the MRHDD on a body surface area basis. Thiazides cross the placental barrier and appear in cord blood. There is a risk of fetal or neonatal jaundice, thrombocytopenia and possibly other adverse reactions that have occurred in adults.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Lisinopril and hydrochlorothiazide is indicated for the treatment of hypertension. These fixed-dose combinations are not indicated for initial therapy (see DOSAGE AND ADMINISTRATION).
In using lisinopril and hydrochlorothiazide, consideration should be given to the fact that an angiotensin converting enzyme inhibitor, captopril, has caused agranulocytosis, particularly in patients with renal impairment or collagen vascular disease, and that available data are insufficient to show that lisinopril does not have a similar risk. (See WARNINGS.)
In considering use of lisinopril and hydrochlorothiazide it should be noted that black patients receiving ACE inhibitors have been reported to have a higher incidence of angioedema compared to non-blacks. (See WARNINGS, Angioedema.)
History
There is currently no drug history available for this drug.
Other Information
Lisinopril and hydrochlorothiazide combines an angiotensin converting enzyme inhibitor, lisinopril and a diuretic, hydrochlorothiazide.
Lisinopril, a synthetic peptide derivative, is an oral long-acting angiotensin converting enzyme inhibitor. It is chemically described as (S)-1-[N2-(1-carboxy-3-phenylpropyl)L-lysyl]-L-proline dihydrate. Its empirical formula is C21H31N305•2H20 and its structural formula is:

Lisinopril is a white to off-white, crystalline powder, with a molecular weight of 441.52. It is soluble in water, sparingly soluble in methanol, and practically insoluble in ethanol.
Hydrochlorothiazide is 6-chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1-dioxide. Its empirical formula is C7H8CIN304S2 and its structural formula is:

Hydrochlorothiazide is a white, or practically white, crystalline powder with a molecular weight of 297.73, which is slightly soluble in water, but freely soluble in sodium hydroxide solution.
Lisinopril and hydrochlorothiazide is available for oral use in three tablet combinations of lisinopril and hydrochlorothiazide: 10-12.5 mg containing 10 mg lisinopril and 12.5 mg hydrochlorothiazide, lisinopril and hydrochlorothiazide: 20-12.5 mg containing 20 mg lisinopril and 12.5 mg hydrochlorothiazide and lisinopril and hydrochlorothiazide: 20-25 mg containing 20 mg lisinopril and 25 mg hydrochlorothiazide.
Inactive ingredients are as follows:
10/12.5 mg: Calcium Phosphate Dibasic, Colloidal Silicon Dioxide, Corn Starch, FD&C Blue #2, Lactose Monohydrate, Magnesium Stearate, Mannitol, and Sodium Starch Glycolate.
20/12.5 mg: Calcium Phosphate Dibasic, Colloidal Silicon Dioxide, Corn Starch, Lactose Monohydrate, Magnesium Stearate, Mannitol, Sodium Starch Glycolate, and Yellow Iron Oxide.
20/25 mg: Calcium Phosphate Dibasic, Colloidal Silicon Dioxide, Corn Starch, Lactose Monohydrate, Magnesium Stearate, Mannitol, Red Iron Oxide, and Sodium Starch Glycolate.
Sources
Lisinopril With Hydrochlorothiazide Manufacturers
-
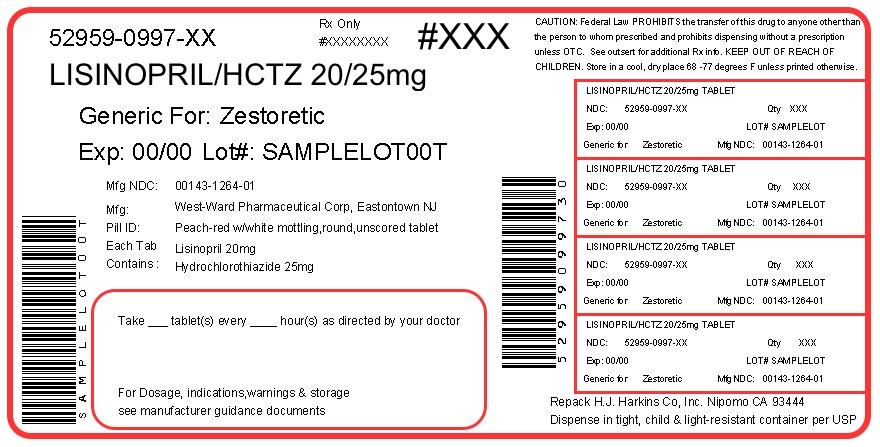
H.j. Harkins Company, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [H.j. Harkins Company, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | H.j. Harkins Company, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [H.j. Harkins Company, Inc.] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [H.j. Harkins Company, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide is effective in doses of 12.5-50 mg. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide will be associated with both sets of dose-independent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-independent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10/12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20/12.5 mg. Further increases of either or both components could depend on clinical response. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen, may achieve similar or greater blood pressure control with less potassium loss if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10/12.5 mg. Dosage higher than lisinopril 80 mg and hydrochlorothiazide 50 mg should not be used.
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentThe usual regimens of therapy with lisinopril and hydrochlorothiazide need not be adjusted as long as the patient's creatinine clearance is >30 mL/min/1.73m2 (serum creatinine approximately ≤3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended (see WARNINGS, Anaphylactoid reactions during membrane exposure).
-
Pd-rx Pharmaceuticals, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | Pd-rx Pharmaceuticals, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentRegimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS, Anaphylactoid reactions during membrane exposure).
-
Golden State Medical Supply, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | Golden State Medical Supply, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Golden State Medical Supply, Inc.] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentRegimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS, Anaphylactoid reactions during membrane exposure).
-
Pd-rx Pharmaceuticals, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | Pd-rx Pharmaceuticals, Inc.
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentRegimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS, Anaphylactoid reactions during membrane exposure).
-
Pd-rx Pharmaceuticals, Inc.
-
Aphena Pharma Solutions – Tennessee, Llc
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | Aphena Pharma Solutions - Tennessee, Llc
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentRegimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS,Anaphylactoid reactions during membrane exposure).
-
Aphena Pharma Solutions – Tennessee, Llc
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | Aphena Pharma Solutions - Tennessee, Llc
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10-80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 - 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10-80 mg and hydrochlorothiazide doses of 6.25-50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose- independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical EffectA patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg or Lisinopril and Hydrochlorothiazide Tablets 20-12.5 mg, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2-3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to Lisinopril and Hydrochlorothiazide Tablets 10-12.5 mg.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension. (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour (see WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of Lisinopril and Hydrochlorothiazide Tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement TherapyThe combination may be substituted for the titrated individual components.
Use in Renal ImpairmentRegimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended(see WARNINGS,Anaphylactoid reactions during membrane exposure).
-
West-ward Pharmaceutical Corp
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [West-ward Pharmaceutical Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril With Hydrochlorothiazide | West-ward Pharmaceutical Corp
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [West-ward Pharmaceutical Corp] Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [West-ward Pharmaceutical Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lisinopril monotherapy is an effective treatment of hypertension in once-daily doses of 10 to 80 mg, while hydrochlorothiazide monotherapy is effective in doses of 12.5 to 50 mg per day. In clinical trials of lisinopril/hydrochlorothiazide combination therapy using lisinopril doses of 10 to 80 mg and hydrochlorothiazide doses of 6.25 to 50 mg, the antihypertensive response rates generally increased with increasing dose of either component.
The side effects (see WARNINGS) of lisinopril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of lisinopril and hydrochlorothiazide may be associated with either or both dose-independent or dose-dependent side effects, but addition of lisinopril in clinical trials blunted the hypokalemia normally seen with diuretics.
To minimize dose-dependent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical Effect:A patient whose blood pressure is not adequately controlled with either lisinopril or hydrochlorothiazide monotherapy may be switched to lisinopril and hydrochlorothiazide tablets 10/12.5 or lisinopril and hydrochlorothiazide tablets 20/12.5, depending on current monotherapy dose. Further increases of either or both components should depend on clinical response with blood pressure measured at the interdosing interval to ensure that there is an adequate antihypertensive effect at that time. The hydrochlorothiazide dose should generally not be increased until 2 to 3 weeks have elapsed. After addition of the diuretic it may be possible to reduce the dose of lisinopril. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen may achieve similar or greater blood-pressure control without electrolyte disturbance if they are switched to lisinopril and hydrochlorothiazide tablets 10/12.5.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally may occur following the initial dose of lisinopril. The diuretic should, if possible, be discontinued for two to three days before beginning therapy with lisinopril to reduce the likelihood of hypotension (See WARNINGS). If the patient’s blood pressure is not controlled with lisinopril alone, diuretic therapy may be resumed.
If the diuretic cannot be discontinued, an initial dose of 5 mg of lisinopril should be used under medical supervision for at least two hours and until blood pressure has stabilized for at least an additional hour See WARNINGS and PRECAUTIONS, Drug Interactions).
Concomitant administration of lisinopril and hydrochlorothiazide tablets with potassium supplements, potassium salt substitutes or potassium-sparing diuretics may lead to increases of serum potassium (See PRECAUTIONS).
Replacement Therapy:The combination may be substituted for the titrated individual components.
Use in Renal Impairment:Regimens of therapy with lisinopril and hydrochlorothiazide need not take account of renal function as long as the patient's creatinine clearance is >30 mL/min/1.7 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 μmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so lisinopril and hydrochlorothiazide is not recommended (See WARNINGS, Anaphylactoid Reactions During Membrane Exposure).
Login To Your Free Account


![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=52be6388-b142-4a4f-8109-99afbbb9f8d8&name=43063065.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Golden State Medical Supply, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c5aa1c63-31c4-49d2-b8f6-6c754dcc0a5c&name=f058b884-c726-4e19-b019-f9f885a028ab-03.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=caa8f69c-2a33-4b0c-baad-725d4112f8f8&name=43063118.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=4374f3e3-7a05-4145-b599-0ce822dff358&name=label.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=ae316da6-4254-4178-ad5a-20b2a2b0024c&name=67544-276.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [Aphena Pharma Solutions – Tennessee, Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=875916f8-fbf2-4db2-b979-088c570377f0&name=43353-800.jpg)
![Lisinopril With Hydrochlorothiazide (Lisinopril And Hydrochlorothiazide) Tablet [West-ward Pharmaceutical Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6573671e-3386-43d0-8f7c-bb8456bdfcbd&name=lisinopril-and-hydrochlorothiazide-3.jpg)