FDA records indicate that there are no current recalls for this drug.
Paxil
Paxil (paroxetine) is an antidepressant medication. It is used to treat anxiety disorders, depression, and hot flashes. It has not been approved for use in children and older adults are more likely to develop serious complications from taking it. Pregnant and breastfeeding women should only take this drug if the benefit exceeds the risk to their newborn.
Are you a medical professional?
Trending Topics
Paxil Recall
In March 2005, US marshals seized lots of Paxil CR from GlaxoSmithKline due to subpar manufacturing standards resulting in poor quality pharmaceutical products. It was discovered that Paxil CR tablets were breaking and were not delivering the correct amount of medication at the correct rate. (fda.gov)
Questions & Answers
Side Effects & Adverse Reactions
People taking this drug have reported mood and behavior changes including panic attacks, aggression, hyperactivity, and suicidal thoughts and behaviors. It can alter the way you think and behave, so be aware of how it affects you before you do anything that is potentially dangerous (like driving).
Methylene blue injection, pimozide, and thioridazine should not be taken with paroxetine. Using a Monoamine oxidase inhibitor (MAOI) within 14 days of starting or stopping this drug is very dangerous. Other common MAOIs are Selegiline, Phenelzine, and Tranylcypromine. Taking Paxil with NSAIDS (non steroidal anti-inflammatory drugs) and other drugs that thin blood can cause individuals to bruise and bleed more than usual. Other medications that cause drowsiness such as muscle relaxants and narcotic pain killers will intensify this effect. Consuming alcohol can increase side effects and is not recommended. This drug can change the way certain medications in your bloodstream work including Coumadin (warfarin) and antipsychotics such as Abilify (aripiprazole) and Risperdal (risperidone).
Paroxetine can cause serious side effects including facial swelling, agitation, trouble sleeping, blurry vision, bone fractures, muscle stiffness, and rash. It can also cause changes in sexual function, trouble breathing, hallucinations, irregular heartbeat, and seizures. You should be cautious when taking it if ulcers, bleeding problems, seizures, liver, or kidney issues run in your family. Older adults taking it are more likely to develop side effects including hyponatremia- a disorder characterized by low blood sodium. Men that plan to have children should use this drug with caution because it can lower sperm count. Paroxetine has not been approved for pediatric use because the effects on children are not well-researched. (webmd.com)
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older. It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1,000 Patients Treated |
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18-24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25-64 | 1 fewer case |
| ≥65 | 6 fewer cases |
Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-like Reactions
This medication has one of the highest rates of withdrawal symptoms among those who stop taking it. SSRIs should never be discontinued abruptly; your dose should be gradually reduced by a doctor. Serotonin syndrome or Neuroleptic Malignant Syndrome (NMS)-like reactions have been reported with SNRIs and SSRIs alone, including treatment with PAXIL, but particularly with concomitant use of serotonergic drugs (including triptans) with drugs which impair metabolism of serotonin (including MAOIs), or with antipsychotics or other dopamine antagonists. Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination) and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Serotonin syndrome, in its most severe form can resemble neuroleptic malignant syndrome, which includes hyperthermia, muscle rigidity, autonomic instability with possible rapid fluctuation of vital signs, and mental status changes. Patients should be monitored for the emergence of serotonin syndrome or NMS-like signs and symptoms. (aafp.org)
Use During Pregnancy
Paxil is labeled as a Category D pregnancy risk and should only be administered to pregnant and nursing women if the benefit to the mother outweighs the risk to the infant. Epidemiological studies have shown that infants exposed in the first trimester of pregnancy have an increased risk of congenital malformations, particularly cardiovascular malformations.
Legal Issues
Several class-action lawsuits have been filed against GlaxoSmithKline, the makers of Paxil, as a result of failing to sufficiently warn consumers of its addictive properties. The same company paid $2.5 million to settle charges of consumer fraud in 2004 for knowingly and systematically withholding unfavorable research findings from consumers. In 2012, they were penalized $3 billion - the largest fine in US healthcare fraud history - resulting from various civil and criminal charges including off-label marketing to treat children.
FDA Safety Alerts
In December 2005, the FDA announced that PAXIL (paroxetine HCl) and PAXIL CR (paroxetine HCl) Controlled-Release Tablets can cause major congenital malformations in infants born to mothers that took the drug during their first trimester of pregnancy. They increased the pregnancy risk category from “C” to “D” - acknowledging the risks of use and the danger to the fetus. (fda.gov)
The FDA issued a public health advisory in May 2014 to alert consumers and healthcare providers of worsening depression in patients with major depressive disorder that take Paxil and other antidepressants. These individuals are at an increased risk of suicidal thoughts and behaviors, especially when starting it or following an increase in dose. Other antidepressants that increase these risks are Zoloft (sertraline), Lexapro (escitalopram), Effexor (venlafaxine), Prozac (fluoxetine), Wellbutrin (bupropion), Remeron (mirtazapine), Luvox (fluvoxamine), Serzone (nefazodone), and Celexa (citalopram). (fda.gov)
Manufacturer Warnings
There are currently no manufacturer warnings for Paxil.
FDA Labeling Changes
July 2014 - Paxil and other drugs used to treat major depressive disorder cause pupillary dilation and may cause an angle closure attack in people with narrow angles who don’t have a patent iridotomy (a treatment for block glaucoma). Taking paroxetine can result in eye pain, eye swelling or redness, and changes in vision. (fda.gov)
December 2012 - Paxil causes Stevens-Johnson Syndrome, a disease of the skin and mucous membranes with flu-like symptoms, painful rash, and blisters. This is a medical emergency that typically requires hospitalization, and it can take months after discontinuing use to recover. (fda.gov)
July 2011 - Patients on a reversible MAOI such as methylene blue or linezolid should not take Paxil, Paxil CR Tablets, or Paxil Oral Suspension due to the increased risk of developing serotonin syndrome, a condition caused by dangerously high levels of the chemical in the brain. Symptoms of serotonin syndrome are diarrhea, fever, shivering, seizures, and stiff muscles and can be fatal if not treated. Individuals taking reversible MAOIs are also at risk for neuroleptic malignant syndrome (NMS), a disorder that also causes stiff muscles and fever, in addition to other symptoms including hypothermia and changes in consciousness. Patients taking pimozide should not take paroxetine. (fda.gov)
March 2011 - The efficacy of tamoxifen (a medication that treats breast cancer) is reduced when taken with Paxil. (fda.gov)
October 2010 - SSRI’s and other antidepressants can result in an increased risk of developing bone fractures and can cause swelling, bruising, and point tenderness (pain felt in response to pressure on a particular area of the body). Paroxetine can also cause restless leg syndrome and infertility in men. (fda.gov)
October 2008 - Drugs metabolized by CYP2D6 (a liver enzyme) such as fluoxetine, risperidone, amitriptyline, type 1C antiarrhythmics (flecainide, propafenone, and encainide), and medications that inhibit this enzyme (including quinidine) may become less effective when taken with Paxil. (fda.gov)
Uses
Paroxetine is an antidepressant medication in the selective serotonin reuptake inhibitor (SSRI) class of drugs. It balances the neurotransmitter serotonin - a chemical in the brain that is believed to affect mood, appetite, energy level, and sleep. It is prescribed to patients suffering from depression, anxiety disorders, premenstrual dysphoric disorder, posttraumatic stress disorder (PTSD), and obsessive-compulsiveness disorder (OCD). This drug is sold in the United States under the brand names Paxil, Paxil CR, Brisdelle, and Pexeva. Other trade names are Aropax (in New Zealand), Deroxat (in France), Sereupin (a derivative that is available worldwide), Paxtine (in Australia), and Paraxyl (in Pakistan). It comes in two forms: tablet (paroxetine HCI) and liquid suspension, ranging from 10 mg to 40 mg per dose. (webmd.com)
History
The British pharmaceutical company GlaxoSmithKline, formerly known as SmithKline Beecham, first marketed Paxil in 1992. Generic versions of the drug became available in 2003, when the patent expired. In 2013, it was approved by the FDA to treat hot flashes associated with menopause.
Other Information
PAXIL (paroxetine hydrochloride) is an orally administered psychotropic drug. It is the hydrochloride salt of a phenylpiperidine compound identified chemically as (-)-trans-4R-(4'-fluorophenyl)-3S-[(3',4'-methylenedioxyphenoxy) methyl] piperidine hydrochloride hemihydrate and has the empirical formula of C19H20FNO3•HCl•1/2H2O. The molecular weight is 374.8 (329.4 as free base). The structural formula of paroxetine hydrochloride is:
 Paroxetine hydrochloride is an odorless, off-white powder, having a melting point range of 120° to 138°C and a solubility of 5.4 mg/mL in water.
Paroxetine hydrochloride is an odorless, off-white powder, having a melting point range of 120° to 138°C and a solubility of 5.4 mg/mL in water.
Tablets
Each film-coated tablet contains paroxetine hydrochloride equivalent to paroxetine as follows: 10 mg–yellow (scored); 20 mg–pink (scored); 30 mg–blue, 40 mg–green. Inactive ingredients consist of dibasic calcium phosphate dihydrate, hypromellose, magnesium stearate, polyethylene glycols, polysorbate 80, sodium starch glycolate, titanium dioxide, and 1 or more of the following: D&C Red No. 30 aluminum lake, D&C Yellow No. 10 aluminum lake, FD&C Blue No. 2 aluminum lake, FD&C Yellow No. 6 aluminum lake.
Suspension for Oral Administration
Each 5 mL of orange-colored, orange-flavored liquid contains paroxetine hydrochloride equivalent to paroxetine, 10 mg. Inactive ingredients consist of polacrilin potassium, microcrystalline cellulose, propylene glycol, glycerin, sorbitol, methylparaben, propylparaben, sodium citrate dihydrate, citric acid anhydrous, sodium saccharin, flavorings, FD&C Yellow No. 6 aluminum lake, and simethicone emulsion, USP.
Sources
Paxil Manufacturers
-
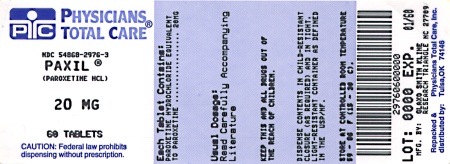
Physicians Total Care, Inc.
![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Paxil | Physicians Total Care, Inc.
![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated [Physicians Total Care, Inc.] Paxil (Paroxetine Hydrochloride) Tablet, Film Coated [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Major Depressive Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended initial dose is 20 mg/day. Patients were dosed in a range of 20 to 50 mg/day in the clinical trials demonstrating the effectiveness of PAXIL in the treatment of major depressive disorder. As with all drugs effective in the treatment of major depressive disorder, the full effect may be delayed. Some patients not responding to a 20-mg dose may benefit from dose increases, in 10-mg/day increments, up to a maximum of 50 mg/day. Dose changes should occur at intervals of at least 1 week.
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. It is generally agreed that acute episodes of major depressive disorder require several months or longer of sustained pharmacologic therapy. Whether the dose needed to induce remission is identical to the dose needed to maintain and/or sustain euthymia is unknown.
Systematic evaluation of the efficacy of PAXIL has shown that efficacy is maintained for periods of up to 1 year with doses that averaged about 30 mg.
Obsessive Compulsive Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended dose of PAXIL in the treatment of OCD is 40 mg daily. Patients should be started on 20 mg/day and the dose can be increased in 10-mg/day increments. Dose changes should occur at intervals of at least 1 week. Patients were dosed in a range of 20 to 60 mg/day in the clinical trials demonstrating the effectiveness of PAXIL in the treatment of OCD. The maximum dosage should not exceed 60 mg/day.
Maintenance TherapyLong-term maintenance of efficacy was demonstrated in a 6-month relapse prevention trial. In this trial, patients with OCD assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGY: Clinical Trials). OCD is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Panic Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The target dose of PAXIL in the treatment of panic disorder is 40 mg/day. Patients should be started on 10 mg/day. Dose changes should occur in 10-mg/day increments and at intervals of at least 1 week. Patients were dosed in a range of 10 to 60 mg/day in the clinical trials demonstrating the effectiveness of PAXIL. The maximum dosage should not exceed 60 mg/day.
Maintenance TherapyLong-term maintenance of efficacy was demonstrated in a 3-month relapse prevention trial. In this trial, patients with panic disorder assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGY: Clinical Trials). Panic disorder is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Social Anxiety Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended and initial dosage is 20 mg/day. In clinical trials the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 60 mg/day. While the safety of PAXIL has been evaluated in patients with social anxiety disorder at doses up to 60 mg/day, available information does not suggest any additional benefit for doses above 20 mg/day (see CLINICAL PHARMACOLOGY: Clinical Trials).
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. Although the efficacy of PAXIL beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, social anxiety disorder is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Generalized Anxiety Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. In clinical trials the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 50 mg/day. The recommended starting dosage and the established effective dosage is 20 mg/day. There is not sufficient evidence to suggest a greater benefit to doses higher than 20 mg/day. Dose changes should occur in 10 mg/day increments and at intervals of at least 1 week.
Maintenance TherapySystematic evaluation of continuing PAXIL for periods of up to 24 weeks in patients with Generalized Anxiety Disorder who had responded while taking PAXIL during an 8-week acute treatment phase has demonstrated a benefit of such maintenance (see CLINICAL PHARMACOLOGY: Clinical Trials). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Posttraumatic Stress Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended starting dosage and the established effective dosage is 20 mg/day. In 1 clinical trial, the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 50 mg/day. However, in a fixed dose study, there was not sufficient evidence to suggest a greater benefit for a dose of 40 mg/day compared to 20 mg/day. Dose changes, if indicated, should occur in 10 mg/day increments and at intervals of at least 1 week.
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. Although the efficacy of PAXIL beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, PTSD is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Special Populations Treatment of Pregnant Women During the Third TrimesterNeonates exposed to PAXIL and other SSRIs or SNRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding (see WARNINGS: Usage in Pregnancy). When treating pregnant women with paroxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment. The physician may consider tapering paroxetine in the third trimester.
Dosage for Elderly or Debilitated Patients, and Patients With Severe Renal or Hepatic ImpairmentThe recommended initial dose is 10 mg/day for elderly patients, debilitated patients, and/or patients with severe renal or hepatic impairment. Increases may be made if indicated. Dosage should not exceed 40 mg/day.
Switching Patients to or From a Monoamine Oxidase Inhibitor AntidepressantAt least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of therapy with PAXIL. Conversely, at least 14 days should be allowed after stopping PAXIL before starting an MAOI antidepressant (see CONTRAINDICATIONS).
Use of PAXIL With Reversible MAOIs Such as Linezolid or Methylene Blue:Do not start PAXIL in a patient who is being treated with linezolid or methylene blue because there is increased risk of serotonin syndrome or NMS-like reactions. In a patient who requires more urgent treatment of a psychiatric condition, non-pharmacological interventions, including hospitalization, should be considered (see CONTRAINDICATIONS). In some cases, a patient receiving therapy with PAXIL may require urgent treatment with linezolid or methylene blue. If acceptable alternatives to linezolid or methylene blue treatment are not available and the potential benefits of linezolid or methylene blue treatment are judged to outweigh the risks of serotonin syndrome or NMS-like reactions in a particular patient, PAXIL should be stopped promptly, and linezolid or methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome or NMS-like reactions for 2 weeks or until 24 hours after the last dose of linezolid or methylene blue, whichever comes first. Therapy with PAXIL may be resumed 24 hours after the last dose of linezolid or methylene blue (see WARNINGS).
Discontinuation of Treatment With PAXILSymptoms associated with discontinuation of PAXIL have been reported (see PRECAUTIONS: Discontinuation of Treatment With PAXIL). Patients should be monitored for these symptoms when discontinuing treatment, regardless of the indication for which PAXIL is being prescribed. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate.
NOTE: SHAKE SUSPENSION WELL BEFORE USING.
-
Apotex Corp
![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated Paxil (Paroxetine Hydrochloride) Suspension [Apotex Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Paxil | Apotex Corp
![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated Paxil (Paroxetine Hydrochloride) Suspension [Apotex Corp] Paxil (Paroxetine Hydrochloride) Tablet, Film Coated Paxil (Paroxetine Hydrochloride) Suspension [Apotex Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Major Depressive Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended initial dose is 20 mg/day. Patients were dosed in a range of 20 to 50 mg/day in the clinical trials demonstrating the effectiveness of PAXIL in the treatment of major depressive disorder. As with all drugs effective in the treatment of major depressive disorder, the full effect may be delayed. Some patients not responding to a 20-mg dose may benefit from dose increases, in 10-mg/day increments, up to a maximum of 50 mg/day. Dose changes should occur at intervals of at least 1 week.
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. It is generally agreed that acute episodes of major depressive disorder require several months or longer of sustained pharmacologic therapy. Whether the dose needed to induce remission is identical to the dose needed to maintain and/or sustain euthymia is unknown.
Systematic evaluation of the efficacy of PAXIL has shown that efficacy is maintained for periods of up to 1 year with doses that averaged about 30 mg.
Obsessive Compulsive Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended dose of PAXIL in the treatment of OCD is 40 mg daily. Patients should be started on 20 mg/day and the dose can be increased in 10-mg/day increments. Dose changes should occur at intervals of at least 1 week. Patients were dosed in a range of 20 to 60 mg/day in the clinical trials demonstrating the effectiveness of PAXIL in the treatment of OCD. The maximum dosage should not exceed 60 mg/day.
Maintenance TherapyLong‑term maintenance of efficacy was demonstrated in a 6‑month relapse prevention trial. In this trial, patients with OCD assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGY: Clinical Trials). OCD is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Panic Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The target dose of PAXIL in the treatment of panic disorder is 40 mg/day. Patients should be started on 10 mg/day. Dose changes should occur in 10-mg/day increments and at intervals of at least 1 week. Patients were dosed in a range of 10 to 60 mg/day in the clinical trials demonstrating the effectiveness of PAXIL. The maximum dosage should not exceed 60 mg/day.
Maintenance TherapyLong-term maintenance of efficacy was demonstrated in a 3‑month relapse prevention trial. In this trial, patients with panic disorder assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGY: Clinical Trials). Panic disorder is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Social Anxiety Disorder: Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended and initial dosage is 20 mg/day. In clinical trials the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 60 mg/day. While the safety of PAXIL has been evaluated in patients with social anxiety disorder at doses up to 60 mg/day, available information does not suggest any additional benefit for doses above 20 mg/day (see CLINICAL PHARMACOLOGY: Clinical Trials).
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. Although the efficacy of PAXIL beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, social anxiety disorder is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Generalized Anxiety Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. In clinical trials the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 50 mg/day. The recommended starting dosage and the established effective dosage is 20 mg/day. There is not sufficient evidence to suggest a greater benefit to doses higher than 20 mg/day. Dose changes should occur in 10 mg/day increments and at intervals of at least 1 week.
Maintenance TherapySystematic evaluation of continuing PAXIL for periods of up to 24 weeks in patients with Generalized Anxiety Disorder who had responded while taking PAXIL during an 8-week acute treatment phase has demonstrated a benefit of such maintenance (see CLINICAL PHARMACOLOGY: Clinical Trials). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Posttraumatic Stress Disorder Usual Initial DosagePAXIL should be administered as a single daily dose with or without food, usually in the morning. The recommended starting dosage and the established effective dosage is 20 mg/day. In 1 clinical trial, the effectiveness of PAXIL was demonstrated in patients dosed in a range of 20 to 50 mg/day. However, in a fixed dose study, there was not sufficient evidence to suggest a greater benefit for a dose of 40 mg/day compared to 20 mg/day. Dose changes, if indicated, should occur in 10 mg/day increments and at intervals of at least 1 week.
Maintenance TherapyThere is no body of evidence available to answer the question of how long the patient treated with PAXIL should remain on it. Although the efficacy of PAXIL beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, PTSD is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Special Populations Treatment of Pregnant Women During the Third TrimesterNeonates exposed to PAXIL and other SSRIs or SNRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding (see WARNINGS: Usage in Pregnancy). When treating pregnant women with paroxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment.
Dosage for Elderly or Debilitated Patients, and Patients With Severe Renal or Hepatic ImpairmentThe recommended initial dose is 10 mg/day for elderly patients, debilitated patients, and/or patients with severe renal or hepatic impairment. Increases may be made if indicated. Dosage should not exceed 40 mg/day.
Switching a Patient to or From a Monoamine Oxidase Inhibitor (MAOI) Intended to Treat Psychiatric DisordersAt least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with PAXIL. Conversely, at least 14 days should be allowed after stopping PAXIL before starting an MAOI intended to treat psychiatric disorders (see CONTRAINDICATIONS).
Use of PAXIL With Other MAOIs, Such as Linezolid or Methylene BlueDo not start PAXIL in a patient who is being treated with linezolid or intravenous methylene blue because there is increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered (see CONTRAINDICATIONS).
In some cases, a patient already receiving therapy with PAXIL may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, PAXIL should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with PAXIL may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue (see WARNINGS).
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with PAXIL is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use (see WARNINGS).
Discontinuation of Treatment With PAXIL:Symptoms associated with discontinuation of PAXIL have been reported (see PRECAUTIONS: Discontinuation of Treatment With PAXIL). Patients should be monitored for these symptoms when discontinuing treatment, regardless of the indication for which PAXIL is being prescribed. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate.
NOTE: SHAKE SUSPENSION WELL BEFORE USING.
Login To Your Free Account




![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated [Physicians Total Care, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=40226242-da82-4dd7-bca2-eebb14501264&name=2976.jpg)
![Paxil (Paroxetine Hydrochloride) Tablet, Film Coated Paxil (Paroxetine Hydrochloride) Suspension [Apotex Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=584ace29-6e40-432f-950f-ab7e98653d32&name=fb260f63-e4ed-4677-b62c-acc42579d19e-02.jpg)