FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Pradaxa Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
There is currently no warning information available for this product. We apologize for any inconvenience.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
PRADAXA is indicated to reduce the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation.
History
There is currently no drug history available for this drug.
Other Information
The chemical name for dabigatran etexilate mesylate, a direct thrombin inhibitor, is β-Alanine, N-[[2-[[[4-[[[(hexyloxy)carbonyl]amino]iminomethyl] phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]carbonyl]-N-2-pyridinyl-,ethyl ester, methanesulfonate. The empirical formula is C34H41N7O5 • CH4O3S and the molecular weight is 723.86 (mesylate salt), 627.75 (free base). The structural formula is:

Dabigatran etexilate mesylate is a yellow-white to yellow powder. A saturated solution in pure water has a solubility of 1.8 mg/mL. It is freely soluble in methanol, slightly soluble in ethanol, and sparingly soluble in isopropanol.
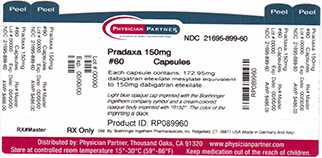
The 150 mg capsule for oral administration contains 172.95 mg dabigatran etexilate mesylate, which is equivalent to 150 mg of dabigatran etexilate, and the following inactive ingredients: acacia, dimethicone, hypromellose, hydroxypropyl cellulose, talc, and tartaric acid. The capsule shell is composed of carrageenan, FD&C Blue No. 2, FD&C Yellow No. 6, hypromellose, potassium chloride, titanium dioxide, and black edible ink. The 75 mg capsule contains 86.48 mg dabigatran etexilate mesylate, equivalent to 75 mg dabigatran etexilate, and is otherwise similar to the 150 mg capsule.
Sources
Pradaxa Manufacturers
-
Rebel Distributors Corp
![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Pradaxa | Rebel Distributors Corp
![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Rebel Distributors Corp] Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 Recommended DoseFor patients with creatinine clearance (CrCl) >30 mL/min, the recommended dose of PRADAXA is 150 mg taken orally, twice daily, with or without food. For patients with CrCl 15-30 mL/min, the recommended dose is 75 mg twice daily [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with a CrCL <15 mL/min or on dialysis cannot be provided.
Instruct patients to swallow the capsules whole. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)].
If a dose of PRADAXA is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of PRADAXA should not be doubled to make up for a missed dose.
2.2 Converting from or to WarfarinWhen converting patients from warfarin therapy to PRADAXA, discontinue warfarin and start PRADAXA when the international normalized ratio (INR) is below 2.0.
When converting from PRADAXA to warfarin, adjust the starting time of warfarin based on creatinine clearance as follows:
For CrCl >50 mL/min, start warfarin 3 days before discontinuing PRADAXA. For CrCl 31-50 mL/min, start warfarin 2 days before discontinuing PRADAXA. For CrCl 15-30 mL/min, start warfarin 1 day before discontinuing PRADAXA. For CrCl <15 mL/min, no recommendations can be made.Because PRADAXA can contribute to an elevated INR, the INR will better reflect warfarin’s effect after PRADAXA has been stopped for at least 2 days.
2.3 Converting from or to Parenteral AnticoagulantsFor patients currently receiving a parenteral anticoagulant, start PRADAXA 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin).
For patients currently taking PRADAXA, wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of PRADAXA before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)].
2.4 Surgery and InterventionsIf possible, discontinue PRADAXA 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.1)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.2)]. Bleeding risk can be assessed by the ecarin clotting time (ECT). This test is a better marker of the anticoagulant activity of dabigatran than activated partial thromboplastin time (aPTT), prothrombin time (PT)/INR, or thrombin time (TT). If ECT is not available, the aPTT test provides an approximation of PRADAXA’s anticoagulant activity [see Clinical Pharmacology (12.2)].
-
Boehringer Ingelheim Pharmaceuticals Inc.
![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Boehringer Ingelheim Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Pradaxa | Boehringer Ingelheim Pharmaceuticals Inc.
![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Boehringer Ingelheim Pharmaceuticals Inc.] Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Boehringer Ingelheim Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 Recommended Dose Indication Dosage Reduction in Risk of Stroke and Systemic Embolism in Non-valvular AF CrCl >30 mL/min:
150 mg twice daily
CrCl 15 to 30 mL/min:
75 mg twice daily
CrCl <15 mL/min or on dialysis:
Dosing recommendations cannot be provided
CrCl 30 to 50 mL/min with concomitant use of P-gp inhibitors:
Reduce dose to 75 mg twice daily if given with P-gp inhibitors dronedarone or systemic ketoconazole.
CrCl <30 mL/min with concomitant use of P-gp inhibitors:
Avoid co-administration
Treatment of DVT and PE
Reduction in the Risk of Recurrence of DVT and PE CrCl >30 mL/min:
150 mg twice daily
CrCl ≤30 mL/min or on dialysis:
Dosing recommendations cannot be provided
CrCl <50 mL/min with concomitant use of P-gp inhibitors:
Avoid co-administration
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation
For patients with creatinine clearance (CrCl) >30 mL/min, the recommended dose of PRADAXA is 150 mg taken orally, twice daily. For patients with severe renal impairment (CrCl 15-30 mL/min), the recommended dose of PRADAXA is 75 mg twice daily [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with a CrCl <15 mL/min or on dialysis cannot be provided.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism
For patients with CrCl >30 mL/min, the recommended dose of PRADAXA is 150 mg taken orally, twice daily, after 5-10 days of parenteral anticoagulation. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism
For patients with CrCl >30 mL/min, the recommended dose of PRADAXA is 150 mg taken orally, twice daily after previous treatment. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.2 Dosing AdjustmentsAssess renal function prior to initiation of treatment with PRADAXA. Periodically assess renal function as clinically indicated (i.e., more frequently in clinical situations that may be associated with a decline in renal function) and adjust therapy accordingly. Discontinue PRADAXA in patients who develop acute renal failure while on PRADAXA and consider alternative anticoagulant therapy.
Generally, the extent of anticoagulation does not need to be assessed. When necessary, use aPTT or ECT, and not INR, to assess for anticoagulant activity in patients on PRADAXA [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation
In patients with moderate renal impairment (CrCl 30-50 mL/min), concomitant use of the P-gp inhibitor dronedarone or systemic ketoconazole can be expected to produce dabigatran exposure similar to that observed in severe renal impairment. Reduce the dose of PRADAXA to 75 mg twice daily [see Warnings and Precautions (5.5), Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism
Dosing recommendations for patients with CrCl ≤30 mL/min cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min [see Warnings and Precautions (5.5), Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
2.3 Instructions to PatientsInstruct patients to swallow the capsules whole. PRADAXA should be taken with a full glass of water. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)].
If a dose of PRADAXA is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of PRADAXA should not be doubled to make up for a missed dose.
2.4 Converting from or to WarfarinWhen converting patients from warfarin therapy to PRADAXA, discontinue warfarin and start PRADAXA when the INR is below 2.0.
When converting from PRADAXA to warfarin, adjust the starting time of warfarin based on creatinine clearance as follows:
For CrCl ≥50 mL/min, start warfarin 3 days before discontinuing PRADAXA. For CrCl 30-50 mL/min, start warfarin 2 days before discontinuing PRADAXA. For CrCl 15-30 mL/min, start warfarin 1 day before discontinuing PRADAXA. For CrCl <15 mL/min, no recommendations can be made.Because PRADAXA can increase INR, the INR will better reflect warfarin’s effect only after PRADAXA has been stopped for at least 2 days [see Clinical Pharmacology (12.2)].
2.5 Converting from or to Parenteral AnticoagulantsFor patients currently receiving a parenteral anticoagulant, start PRADAXA 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin).
For patients currently taking PRADAXA, wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of PRADAXA before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)].
2.6 Discontinuation for Surgery and Other InterventionsIf possible, discontinue PRADAXA 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.2)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.1, 5.3)].
Login To Your Free Account


![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Rebel Distributors Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5db7f199-8752-4d24-85f7-e34ca8f4d02e&name=5db7f199-8752-4d24-85f7-e34ca8f4d02e-04.jpg)
![Pradaxa (Dabigatran Etexilate Mesylate) Capsule [Boehringer Ingelheim Pharmaceuticals Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=ba74e3cd-b06f-4145-b284-5fd6b84ff3c9&name=carton013512.jpg)