FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Sotalol Hydrochloride Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
The National Heart, Lung, and Blood Institute’s Cardiac Arrhythmia Suppression Trial I (CAST I) was a long-term, multi-center, double-blind study in patients with asymptomatic, non-life-threatening ventricular arrhythmias, 1 to 103 weeks after acute myocardial infarction. Patients in CAST I were randomized to receive placebo or individually optimized doses of encainide, flecainide, or moricizine. The Cardiac Arrhythmia Suppression Trial II (CAST II) was similar, except that the recruited patients had had their index infarction 4 to 90 days before randomization, patients with left ventricular ejection fractions greater than 40% were not admitted, and the randomized regimens were limited to placebo and moricizine.
CAST I was discontinued after an average time-on-treatment of 10 months, and CAST II was discontinued after an average time-on-treatment of 18 months. As compared to placebo treatment, all three active therapies were associated with increases in short-term (14-day) mortality, and encainide and flecainide were associated with significant increases in longer-term mortality as well. The longer-term mortality rate associated with moricizine treatment could not be statistically distinguished from that associated with placebo.
The applicability of these results to other populations (e.g., those without recent myocardial infarction) and to other than Class I antiarrhythmic agents is uncertain. Sotalol hydrochloride is devoid of Class I effects, and in a large (n = 1,456) controlled trial in patients with a recent myocardial infarction, who did not necessarily have ventricular arrhythmias, sotalol hydrochloride did not produce increased mortality at doses up to 320 mg/day (see Clinical Studies). On the other hand, in the large post-infarction study using a non-titrated initial dose of 320 mg once daily and in a second small randomized trial in high-risk post-infarction patients treated with high doses (320 mg BID), there have been suggestions of an excess of early sudden deaths.
Like other antiarrhythmic agents, sotalol can provoke new or worsened ventricular arrhythmias in some patients, including sustained ventricular tachycardia or ventricular fibrillation, with potentially fatal consequences. Because of its effect on cardiac repolarization (QTc interval prolongation), torsade de pointes, a polymorphic ventricular tachycardia with prolongation of the QT interval and a shifting electrical axis is the most common form of proarrhythmia associated with sotalol, occurring in about 4% of high risk (history of sustained VT/VF) patients. The risk of torsade de pointes progressively increases with prolongation of the QT interval, and is worsened also by reduction in heart rate and reduction in serum potassium (see Electrolyte Disturbances).
Because of the variable temporal recurrence of arrhythmias, it is not always possible to distinguish between a new or aggravated arrhythmic event and the patient's underlying rhythm disorder. (Note, however, that torsade de pointes is usually a drug-induced arrhythmia in people with an initially normal QTc.) Thus, the incidence of drug-related events cannot be precisely determined, so that the occurrence rates provided must be considered approximations. Note also that drug-induced arrhythmias may often not be identified, particularly if they occur long after starting the drug, due to less frequent monitoring. It is clear from the NIH-sponsored CAST (see WARNINGS: Mortality) that some antiarrhythmic drugs can cause increased sudden death mortality, presumably due to new arrhythmias or asystole, that do not appear early in treatment but that represent a sustained increased risk.
Overall in clinical trials with sotalol, 4.3% of 3257 patients experienced a new or worsened ventricular arrhythmia. Of this 4.3%, there was new or worsened sustained ventricular tachycardia in approximately 1% of patients and torsade de pointes in 2.4%. Additionally, in approximately 1% of patients, deaths were considered possibly drug-related; such cases, although difficult to evaluate, may have been associated with proarrhythmic events. In patients with a history of sustained ventricular tachycardia, the incidence of torsade de pointes was 4% and worsened VT in about 1%; in patients with other, less serious, ventricular arrhythmias and supraventricular arrhythmias, the incidence of torsade de pointes was 1% and 1.4%, respectively.
Torsade de pointes arrhythmias were dose related, as is the prolongation of QT (QTc) interval, as shown in the table below.
| Daily Dose (mg) |
Incidence of Torsade de Pointes |
Mean QTca (msec) |
| 80 |
0 (69)b |
463 (17) |
| 160 |
0.5 (832) |
467 (181) |
| 320 |
1.6 (835) |
473 (344) |
| 480 |
4.4 (459) |
483 (234) |
| 640 |
3.7 (324) |
490 (185) |
| >640 |
5.8 (103) |
512 (62) |
aHighest on-therapy value
bNumber of patients assessed
In addition to dose and presence of sustained VT, other risk factors for torsade de pointes were gender (females had a higher incidence), excessive prolongation of the QTc interval (see table below) and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure appear to have the highest risk for serious proarrhythmia (7%). Of the patients experiencing torsade de pointes, approximately two-thirds spontaneously reverted to their baseline rhythm. The others were either converted electrically (D/C cardioversion or overdrive pacing) or treated with other drugs (see OVERDOSAGE). It is not possible to determine whether some sudden deaths represented episodes of torsade de pointes, but in some instances sudden death did follow a documented episode of torsade de pointes. Although sotalol therapy was discontinued in most patients experiencing torsade de pointes, 17% were continued on a lower dose.
Nonetheless, sotalol should be used with particular caution if the QTc is greater than 500 msec on-therapy and serious consideration should be given to reducing the dose or discontinuing therapy when the QTc exceeds 550 msec. Due to the multiple risk factors associated with torsade de pointes, however, caution should be exercised regardless of the QTc interval. The table below relates the incidence of torsade de pointes to on-therapy QTc and change in QTc from baseline. It should be noted, however, that the highest on-therapy QTc was in many cases the one obtained at the time of the torsade de pointes event, so that the table overstates the predictive value of a high QTc.
| On-Therapy QTc Interval (msec) |
Incidence of Torsade de Pointes |
Change in QTc Interval From Baseline (msec) |
Incidence of Torsade de Pointes |
| <500 |
1.3% (1787) |
<65 |
1.6% (1516) |
| 500 to 525 |
3.4% (236) |
65 to 80 |
3.2% (158) |
| 525 to 550 |
5.6% (125) |
80 to 100 |
4.1% (146) |
| >550 |
10.8% (157) |
100 to 130 |
5.2% (115) |
|
|
|
>130 |
7.1% (99) |
( ) Number of patients assessed
Proarrhythmic events must be anticipated not only on initiating therapy, but with every upward dose adjustment. Proarrhythmic events most often occur within 7 days of initiating therapy or of an increase in dose; 75% of serious proarrhythmias (torsade de pointes and worsened VT) occurred within 7 days of initiating sotalol therapy, while 60% of such events occurred within 3 days of initiation or a dosage change. Initiating therapy at 80 mg BID with gradual upward dose titration and appropriate evaluations for efficacy (e.g., PES or Holter) and safety (e.g., QT interval, heart rate and electrolytes) prior to dose escalation, should reduce the risk of proarrhythmia. Avoiding excessive accumulation of sotalol in patients with diminished renal function, by appropriate dose reduction, should also reduce the risk of proarrhythmia (see DOSAGE AND ADMINISTRATION).
Sympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta-blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In patients who have congestive heart failure controlled by digitalis and/or diuretics, sotalol should be administered cautiously. Both digitalis and sotalol slow AV conduction. As with all beta-blockers, caution is advised when initiating therapy in patients with any evidence of left ventricular dysfunction. In premarketing studies, new or worsened congestive heart failure (CHF) occurred in 3.3% (n = 3257) of patients and led to discontinuation in approximately 1% of patients receiving sotalol. The incidence was higher in patients presenting with sustained ventricular tachycardia/fibrillation (4.6%, n = 1363), or a prior history of heart failure (7.3%, n = 696). Based on a life-table analysis, the one-year incidence of new or worsened CHF was 3% in patients without a prior history and 10% in patients with a prior history of CHF. NYHA Classification was also closely associated to the incidence of new or worsened heart failure while receiving sotalol (1.8% in 1395 Class I patients, 4.9% in 1254 Class II patients and 6.1% in 278 Class III or IV patients).
Sotalol should not be used in patients with hypokalemia or hypomagnesemia prior to correction of imbalance, as these conditions can exaggerate the degree of QT prolongation, and increase the potential for torsade de pointes. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or patients receiving concomitant diuretic drugs.
Excessive prolongation of the QT interval (>550 msec) can promote serious arrhythmias and should be avoided (see Proarrhythmia above). Sinus bradycardia (heart rate less than 50 bpm) occurred in 13% of patients receiving sotalol in clinical trials, and led to discontinuation in about 3% of patients. Bradycardia itself increases the risk of torsade de pointes. Sinus pause, sinus arrest and sinus node dysfunction occur in less than 1% of patients. The incidence of 2nd- or 3rd-degree AV block is approximately 1%.
Sotalol can be used safely and effectively in the long-term treatment of life-threatening ventricular arrhythmias following a myocardial infarction. However, experience in the use of sotalol to treat cardiac arrhythmias in the early phase of recovery from acute MI is limited and at least at high initial doses is not reassuring (see WARNINGS: Mortality). In the first 2 weeks post-MI caution is advised and careful dose titration is especially important, particularly in patients with markedly impaired ventricular function.
The following warnings are related to the beta-blocking activity of sotalol.
Hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy. Occasional cases of exacerbation of angina pectoris, arrhythmias and, in some cases, myocardial infarction have been reported after abrupt discontinuation of beta-blocker therapy. Therefore, it is prudent when discontinuing chronically administered sotalol, particularly in patients with ischemic heart disease, to carefully monitor the patient and consider the temporary use of an alternate beta-blocker if appropriate. If possible, the dosage of sotalol hydrochloride should be gradually reduced over a period of one to two weeks. If angina or acute coronary insufficiency develops, appropriate therapy should be instituted promptly. Patients should be warned against interruption or discontinuation of therapy without the physician's advice. Because coronary artery disease is common and may be unrecognized in patients receiving sotalol, abrupt discontinuation in patients with arrhythmias may unmask latent coronary insufficiency.
PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD IN GENERAL NOT RECEIVE BETA-BLOCKERS. It is prudent, if sotalol hydrochloride is to be administered, to use the smallest effective dose, so that inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of beta2 receptors may be minimized.
While taking beta-blockers, patients with a history of anaphylactic reaction to a variety of allergens may have a more severe reaction on repeated challenge, either accidental, diagnostic or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat the allergic reaction.
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
In patients with diabetes (especially labile diabetes) or with a history of episodes of spontaneous hypoglycemia, sotalol should be given with caution since beta-blockade may mask some important premonitory signs of acute hypoglycemia; e.g., tachycardia.
Sotalol should be used only with extreme caution in patients with sick sinus syndrome associated with symptomatic arrhythmias, because it may cause sinus bradycardia, sinus pauses or sinus arrest.
Beta-blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-blockade which might be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm.
The National Heart, Lung, and Blood Institute’s Cardiac Arrhythmia Suppression Trial I (CAST I) was a long-term, multi-center, double-blind study in patients with asymptomatic, non-life-threatening ventricular arrhythmias, 1 to 103 weeks after acute myocardial infarction. Patients in CAST I were randomized to receive placebo or individually optimized doses of encainide, flecainide, or moricizine. The Cardiac Arrhythmia Suppression Trial II (CAST II) was similar, except that the recruited patients had had their index infarction 4 to 90 days before randomization, patients with left ventricular ejection fractions greater than 40% were not admitted, and the randomized regimens were limited to placebo and moricizine.
CAST I was discontinued after an average time-on-treatment of 10 months, and CAST II was discontinued after an average time-on-treatment of 18 months. As compared to placebo treatment, all three active therapies were associated with increases in short-term (14-day) mortality, and encainide and flecainide were associated with significant increases in longer-term mortality as well. The longer-term mortality rate associated with moricizine treatment could not be statistically distinguished from that associated with placebo.
The applicability of these results to other populations (e.g., those without recent myocardial infarction) and to other than Class I antiarrhythmic agents is uncertain. Sotalol hydrochloride is devoid of Class I effects, and in a large (n = 1,456) controlled trial in patients with a recent myocardial infarction, who did not necessarily have ventricular arrhythmias, sotalol hydrochloride did not produce increased mortality at doses up to 320 mg/day (see Clinical Studies). On the other hand, in the large post-infarction study using a non-titrated initial dose of 320 mg once daily and in a second small randomized trial in high-risk post-infarction patients treated with high doses (320 mg BID), there have been suggestions of an excess of early sudden deaths.
ProarrhythmiaLike other antiarrhythmic agents, sotalol can provoke new or worsened ventricular arrhythmias in some patients, including sustained ventricular tachycardia or ventricular fibrillation, with potentially fatal consequences. Because of its effect on cardiac repolarization (QTc interval prolongation), torsade de pointes, a polymorphic ventricular tachycardia with prolongation of the QT interval and a shifting electrical axis is the most common form of proarrhythmia associated with sotalol, occurring in about 4% of high risk (history of sustained VT/VF) patients. The risk of torsade de pointes progressively increases with prolongation of the QT interval, and is worsened also by reduction in heart rate and reduction in serum potassium (see Electrolyte Disturbances).
Because of the variable temporal recurrence of arrhythmias, it is not always possible to distinguish between a new or aggravated arrhythmic event and the patient's underlying rhythm disorder. (Note, however, that torsade de pointes is usually a drug-induced arrhythmia in people with an initially normal QTc.) Thus, the incidence of drug-related events cannot be precisely determined, so that the occurrence rates provided must be considered approximations. Note also that drug-induced arrhythmias may often not be identified, particularly if they occur long after starting the drug, due to less frequent monitoring. It is clear from the NIH-sponsored CAST (see WARNINGS: Mortality) that some antiarrhythmic drugs can cause increased sudden death mortality, presumably due to new arrhythmias or asystole, that do not appear early in treatment but that represent a sustained increased risk.
Overall in clinical trials with sotalol, 4.3% of 3257 patients experienced a new or worsened ventricular arrhythmia. Of this 4.3%, there was new or worsened sustained ventricular tachycardia in approximately 1% of patients and torsade de pointes in 2.4%. Additionally, in approximately 1% of patients, deaths were considered possibly drug-related; such cases, although difficult to evaluate, may have been associated with proarrhythmic events. In patients with a history of sustained ventricular tachycardia, the incidence of torsade de pointes was 4% and worsened VT in about 1%; in patients with other, less serious, ventricular arrhythmias and supraventricular arrhythmias, the incidence of torsade de pointes was 1% and 1.4%, respectively.
Torsade de pointes arrhythmias were dose related, as is the prolongation of QT (QTc) interval, as shown in the table below.
| Daily Dose (mg) |
Incidence of Torsade de Pointes |
Mean QTca (msec) |
| 80 |
0 (69)b |
463 (17) |
| 160 |
0.5 (832) |
467 (181) |
| 320 |
1.6 (835) |
473 (344) |
| 480 |
4.4 (459) |
483 (234) |
| 640 |
3.7 (324) |
490 (185) |
| >640 |
5.8 (103) |
512 (62) |
aHighest on-therapy value
bNumber of patients assessed
In addition to dose and presence of sustained VT, other risk factors for torsade de pointes were gender (females had a higher incidence), excessive prolongation of the QTc interval (see table below) and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure appear to have the highest risk for serious proarrhythmia (7%). Of the patients experiencing torsade de pointes, approximately two-thirds spontaneously reverted to their baseline rhythm. The others were either converted electrically (D/C cardioversion or overdrive pacing) or treated with other drugs (see OVERDOSAGE). It is not possible to determine whether some sudden deaths represented episodes of torsade de pointes, but in some instances sudden death did follow a documented episode of torsade de pointes. Although sotalol therapy was discontinued in most patients experiencing torsade de pointes, 17% were continued on a lower dose.
Nonetheless, sotalol should be used with particular caution if the QTc is greater than 500 msec on-therapy and serious consideration should be given to reducing the dose or discontinuing therapy when the QTc exceeds 550 msec. Due to the multiple risk factors associated with torsade de pointes, however, caution should be exercised regardless of the QTc interval. The table below relates the incidence of torsade de pointes to on-therapy QTc and change in QTc from baseline. It should be noted, however, that the highest on-therapy QTc was in many cases the one obtained at the time of the torsade de pointes event, so that the table overstates the predictive value of a high QTc.
| On-Therapy QTc Interval (msec) |
Incidence of Torsade de Pointes |
Change in QTc Interval From Baseline (msec) |
Incidence of Torsade de Pointes |
| <500 |
1.3% (1787) |
<65 |
1.6% (1516) |
| 500 to 525 |
3.4% (236) |
65 to 80 |
3.2% (158) |
| 525 to 550 |
5.6% (125) |
80 to 100 |
4.1% (146) |
| >550 |
10.8% (157) |
100 to 130 |
5.2% (115) |
|
|
|
>130 |
7.1% (99) |
( ) Number of patients assessed
Proarrhythmic events must be anticipated not only on initiating therapy, but with every upward dose adjustment. Proarrhythmic events most often occur within 7 days of initiating therapy or of an increase in dose; 75% of serious proarrhythmias (torsade de pointes and worsened VT) occurred within 7 days of initiating sotalol therapy, while 60% of such events occurred within 3 days of initiation or a dosage change. Initiating therapy at 80 mg BID with gradual upward dose titration and appropriate evaluations for efficacy (e.g., PES or Holter) and safety (e.g., QT interval, heart rate and electrolytes) prior to dose escalation, should reduce the risk of proarrhythmia. Avoiding excessive accumulation of sotalol in patients with diminished renal function, by appropriate dose reduction, should also reduce the risk of proarrhythmia (see DOSAGE AND ADMINISTRATION).
Congestive Heart FailureSympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta-blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In patients who have congestive heart failure controlled by digitalis and/or diuretics, sotalol should be administered cautiously. Both digitalis and sotalol slow AV conduction. As with all beta-blockers, caution is advised when initiating therapy in patients with any evidence of left ventricular dysfunction. In premarketing studies, new or worsened congestive heart failure (CHF) occurred in 3.3% (n = 3257) of patients and led to discontinuation in approximately 1% of patients receiving sotalol. The incidence was higher in patients presenting with sustained ventricular tachycardia/fibrillation (4.6%, n = 1363), or a prior history of heart failure (7.3%, n = 696). Based on a life-table analysis, the one-year incidence of new or worsened CHF was 3% in patients without a prior history and 10% in patients with a prior history of CHF. NYHA Classification was also closely associated to the incidence of new or worsened heart failure while receiving sotalol (1.8% in 1395 Class I patients, 4.9% in 1254 Class II patients and 6.1% in 278 Class III or IV patients).
Electrolyte DisturbancesSotalol should not be used in patients with hypokalemia or hypomagnesemia prior to correction of imbalance, as these conditions can exaggerate the degree of QT prolongation, and increase the potential for torsade de pointes. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or patients receiving concomitant diuretic drugs.
Conduction DisturbancesExcessive prolongation of the QT interval (>550 msec) can promote serious arrhythmias and should be avoided (see Proarrhythmia above). Sinus bradycardia (heart rate less than 50 bpm) occurred in 13% of patients receiving sotalol in clinical trials, and led to discontinuation in about 3% of patients. Bradycardia itself increases the risk of torsade de pointes. Sinus pause, sinus arrest and sinus node dysfunction occur in less than 1% of patients. The incidence of 2nd- or 3rd-degree AV block is approximately 1%.
Recent Acute MISotalol can be used safely and effectively in the long-term treatment of life-threatening ventricular arrhythmias following a myocardial infarction. However, experience in the use of sotalol to treat cardiac arrhythmias in the early phase of recovery from acute MI is limited and at least at high initial doses is not reassuring (see WARNINGS: Mortality). In the first 2 weeks post-MI caution is advised and careful dose titration is especially important, particularly in patients with markedly impaired ventricular function.
The following warnings are related to the beta-blocking activity of sotalol.
Abrupt WithdrawalHypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy. Occasional cases of exacerbation of angina pectoris, arrhythmias and, in some cases, myocardial infarction have been reported after abrupt discontinuation of beta-blocker therapy. Therefore, it is prudent when discontinuing chronically administered sotalol, particularly in patients with ischemic heart disease, to carefully monitor the patient and consider the temporary use of an alternate beta-blocker if appropriate. If possible, the dosage of sotalol hydrochloride should be gradually reduced over a period of one to two weeks. If angina or acute coronary insufficiency develops, appropriate therapy should be instituted promptly. Patients should be warned against interruption or discontinuation of therapy without the physician's advice. Because coronary artery disease is common and may be unrecognized in patients receiving sotalol, abrupt discontinuation in patients with arrhythmias may unmask latent coronary insufficiency.
Non-Allergic Bronchospasm (e.g., chronic bronchitis and emphysema)PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD IN GENERAL NOT RECEIVE BETA-BLOCKERS. It is prudent, if sotalol hydrochloride is to be administered, to use the smallest effective dose, so that inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of beta2 receptors may be minimized.
AnaphylaxisWhile taking beta-blockers, patients with a history of anaphylactic reaction to a variety of allergens may have a more severe reaction on repeated challenge, either accidental, diagnostic or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat the allergic reaction.
Major SurgeryChronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
DiabetesIn patients with diabetes (especially labile diabetes) or with a history of episodes of spontaneous hypoglycemia, sotalol should be given with caution since beta-blockade may mask some important premonitory signs of acute hypoglycemia; e.g., tachycardia.
Sick Sinus SyndromeSotalol should be used only with extreme caution in patients with sick sinus syndrome associated with symptomatic arrhythmias, because it may cause sinus bradycardia, sinus pauses or sinus arrest.
ThyrotoxicosisBeta-blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-blockade which might be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Oral sotalol hydrochloride is indicated for the treatment of documented ventricular arrhythmias, such as sustained ventricular tachycardia, that in the judgment of the physician are life-threatening. Because of the proarrhythmic effects of sotalol (see WARNINGS), including a 1.5 to 2% rate of torsade de pointes or new VT/VF in patients with either NSVT or supraventricular arrhythmias, its use in patients with less severe arrhythmias, even if the patients are symptomatic, is generally not recommended. Treatment of patients with asymptomatic ventricular premature contractions should be avoided.
Initiation of sotalol treatment or increasing doses, as with other antiarrhythmic agents used to treat life-threatening arrhythmias, should be carried out in the hospital. The response to treatment should then be evaluated by a suitable method (e.g., PES or Holter monitoring) prior to continuing the patient on chronic therapy. Various approaches have been used to determine the response to antiarrhythmic therapy, including sotalol.
In the ESVEM Trial, response by Holter monitoring was tentatively defined as 100% suppression of ventricular tachycardia, 90% suppression of non-sustained VT, 80% suppression of paired VPCs, and 75% suppression of total VPCs in patients who had at least 10 VPCs/hour at baseline; this tentative response was confirmed if VT lasting 5 or more beats was not observed during treadmill exercise testing using a standard Bruce protocol. The PES protocol utilized a maximum of three extrastimuli at three pacing cycle lengths and two right ventricular pacing sites. Response by PES was defined as prevention of induction of the following: 1) monomorphic VT lasting over 15 seconds; 2) non-sustained polymorphic VT containing more than 15 beats of monomorphic VT in patients with a history of monomorphic VT; 3) polymorphic VT or VF greater than 15 beats in patients with VF or a history of aborted sudden death without monomorphic VT; and 4) two episodes of polymorphic VT or VF of greater than 15 beats in a patient presenting with monomorphic VT. Sustained VT or NSVT producing hypotension during the final treadmill test was considered a drug failure.
In a multicenter open-label long-term study of sotalol in patients with life-threatening ventricular arrhythmias which had proven refractory to other antiarrhythmic medications, response by Holter monitoring was defined as in ESVEM. Response by PES was defined as non-inducibility of sustained VT by at least double extrastimuli delivered at a pacing cycle length of 400 msec. Overall survival and arrhythmia recurrence rates in this study were similar to those seen in ESVEM, although there was no comparative group to allow a definitive assessment of outcome.
Antiarrhythmic drugs have not been shown to enhance survival in patients with ventricular arrhythmias.
Sotalol is also indicated for the maintenance of normal sinus rhythm [delay in time to recurrence of atrial fibrillation/atrial flutter (AFIB/AFL)] in patients with symptomatic AFIB/AFL who are currently in sinus rhythm and is marketed under the brand name Betapace AF®. Sotalol Hydrochloride Tablets are not approved for the AFIB/AFL indication and should not be substituted for Betapace AF® because only Betapace AF® is distributed with a patient package insert that is appropriate for patients with AFIB/AFL.
History
There is currently no drug history available for this drug.
Other Information
Sotalol hydrochloride is an antiarrhythmic drug with Class II (beta-adrenoreceptor blocking) and Class III (cardiac action potential duration prolongation) properties. It is supplied as a light-blue, capsule-shaped tablet for oral administration. Sotalol hydrochloride is a white, crystalline solid with a molecular weight of 308.8. It is hydrophilic, soluble in water, propylene glycol and ethanol, but is only slightly soluble in chloroform. Chemically, sotalol hydrochloride is d,l-N-[4-[1-hydroxy-2-[(1-methylethyl)amino]ethyl]phenyl]methane-sulfonamide monohydrochloride. The molecular formula is C12H20N2O3S•HCl and is represented by the following structural formula:
Sources
Sotalol Hydrochloride Manufacturers
-
Proficient Rx Lp
![Sotalol Hydrochloride Tablet [Proficient Rx Lp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Proficient Rx Lp
![Sotalol Hydrochloride Tablet [Proficient Rx Lp] Sotalol Hydrochloride Tablet [Proficient Rx Lp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE ). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE ), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/minDosinga
Interval
(hours)>60
12
30 to 59
24
10 to 29
36 to 48
<10
Dose should be individualized
aThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
1. Measure 120 mL of Simple Syrup. 2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. 3. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. 4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. 5. Allow the tablets to hydrate for at least two hours. 6. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/minDosinga
Interval
(hours)>60
12
30 to 59
24
10 to 29
36 to 48
<10
Dose should be individualized
aThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/minDosinga
Interval
(hours)>60
12
30 to 59
24
10 to 29
36 to 48
<10
Dose should be individualized
aThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
1. Measure 120 mL of Simple Syrup. 2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. 3. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. 4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. 5. Allow the tablets to hydrate for at least two hours. 6. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Global Pharmaceuticals
![Sotalol Hydrochloride Tablet [Global Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Global Pharmaceuticals
![Sotalol Hydrochloride Tablet [Global Pharmaceuticals] Sotalol Hydrochloride Tablet [Global Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
PediatricsPediatric dosing information for sotalol hydrochloride tablets is approved for the Berlex Laboratories sotalol hydrochloride tablets. However, due to the Berlex marketing exclusivity rights, this drug product is not labeled for pediatric use.
-
Rebel Distributors Corp
![Sotalol Hydrochloride Tablet [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Rebel Distributors Corp
![Sotalol Hydrochloride Tablet [Rebel Distributors Corp] Sotalol Hydrochloride Tablet [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE) and the dosage of sotalol hydrochloride tablets must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 mg/day or 320 mg/day (120 mg to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 mg/day to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 mg/day to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater: With normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger: The above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)= 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults, sotalol hydrochloride tablets should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage In Renal ImpairmentAdults: Because sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance Dosing* Interval mL/min (hours) >60 12 30 - 59 24 10 - 29 36 - 48 <10 Dose should be individualized*The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride tablets has increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above).
Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
Children: The use of sotalol hydrochloride tablets in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride TabletsBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see PRECAUTIONS, Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCl. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCl (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity.
Transfer to BETAPACETM AF from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus rhythm should be transferred to BETAPACE AFTM because of the significant differences in labeling (i.e., patient package insert for BETAPACE AFTM, dosing administration and safety information).
-
Pd-rx Pharmaceuticals, Inc.
![Sotalol Hydrochloride Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Pd-rx Pharmaceuticals, Inc.
![Sotalol Hydrochloride Tablet [Pd-rx Pharmaceuticals, Inc.] Sotalol Hydrochloride Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE) and the dosage of sotalol hydrochloride tablets must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 mg/day or 320 mg/day (120 mg to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 mg/day to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 mg/day to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater: With normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger: The above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)= 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults, sotalol hydrochloride tablets should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage In Renal ImpairmentAdults: Because sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance Dosing* Interval mL/min (hours) >60 12 30 - 59 24 10 - 29 36 - 48 <10 Dose should be individualized*The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride tablets has increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above).
Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
Children: The use of sotalol hydrochloride tablets in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride TabletsBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see PRECAUTIONS, Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCl. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCl (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity.
Transfer to BETAPACETM AF from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus rhythm should be transferred to BETAPACE AFTM because of the significant differences in labeling (i.e., patient package insert for BETAPACE AFTM, dosing administration and safety information).
-
Qualitest Pharmaceuticals
![Sotalol Hydrochloride Tablet [Qualitest Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Qualitest Pharmaceuticals
![Sotalol Hydrochloride Tablet [Qualitest Pharmaceuticals] Sotalol Hydrochloride Tablet [Qualitest Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20° to 25°C/68° to 77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20° to 25°C/68° to 77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Apotex Corp.
![Sotalol Hydrochloride Tablet [Apotex Corp.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Apotex Corp.
![Sotalol Hydrochloride Tablet [Apotex Corp.] Sotalol Hydrochloride Tablet [Apotex Corp.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets, USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets, USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets, USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets, USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater
For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steadystate plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger
For children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)=20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults Betapace (sotalol hydrochloride) should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
CreatinineClearance
mL/min
DosingaInterval
(hours)
>60 12 30-59 24 10-29 36-48 <10 Dose should be individualizeda) The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets, USPBefore starting sotalol hydrochloride tablets, USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets, USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionInformation relating to the preparation of an extemporaneous oral solution of sotalol is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled with that information.
Transfer to Betapace AF from Sotalol Hydrochloride Tablets, USPPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets, USP for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Physicians Total Care, Inc.
![Sotalol Hydrochloride Tablet [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Physicians Total Care, Inc.
![Sotalol Hydrochloride Tablet [Physicians Total Care, Inc.] Sotalol Hydrochloride Tablet [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE) and the dosage of sotalol hydrochloride tablets must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 mg/day or 320 mg/day (120 mg to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 mg/day to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 mg/day to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater: With normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger: The above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)= 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults, sotalol hydrochloride tablets should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage In Renal ImpairmentAdults: Because sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance Dosing* Interval mL/min (hours) >60 12 30 - 59 24 10 - 29 36 - 48 <10 Dose should be individualized*The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride tablets has increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above).
Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
Children: The use of sotalol hydrochloride tablets in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride TabletsBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see PRECAUTIONS, Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCl. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCl (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity.
Transfer to BETAPACETM AF from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus rhythm should be transferred to BETAPACE AFTM because of the significant differences in labeling (i.e., patient package insert for BETAPACE AFTM, dosing administration and safety information).
-
Golden State Medical Supply, Inc.
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Golden State Medical Supply, Inc.
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.] Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets, USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets, USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets, USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets, USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
PediatricsPediatric dosing information for sotalol hydrochloride tablets is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled for pediatric use.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30-59 24 10-29 36-48 <10 Dose should be individualizeda) The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets, USPBefore starting sotalol hydrochloride tablets, USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets, USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionInformation relating to the preparation of an extemporaneous oral solution of sotalol is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled with that information.
Transfer to Betapace AF from Sotalol Hydrochloride Tablets, USPPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets, USP for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs] Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Apotex Corp.
![Sotalol Hydrochloride Tablet [Apotex Corp.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Apotex Corp.
![Sotalol Hydrochloride Tablet [Apotex Corp.] Sotalol Hydrochloride Tablet [Apotex Corp.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing and Administration in Adults Therapy with sotalol hydrochloride tablets (AF) must be initiated (and, if necessary, titrated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of 3 days on the maintenance dose. In addition, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm. The QT interval is used to determine patient eligibility for sotalol hydrochloride tablet (AF) treatment and for monitoring safety during treatment. The baseline QT interval must be ≤450 msec in order for a patient to be started on sotalol hydrochloride tablet (AF) therapy. During initiation and titration, the QT interval should be monitored 2 to 4 hours after each dose. If the QT interval prolongs to 500 msec or greater, the dose must be reduced or the drug discontinued. The dose of Sotalol Hydrochloride Tablets, USP (AF) must be individualized according to calculated creatinine clearance. In patients with a creatinine clearance >60 mL/min Sotalol Hydrochloride Tablets, USP (AF) is administered twice daily (BID) while in those with a creatinine clearance between 40 and 60 mL/min, the dose is administered once daily (QD). In patients with a creatinine clearance less than 40 mL/min Sotalol Hydrochloride Tablets, USP (AF) is contraindicated. The recommended initial dose of Sotalol Hydrochloride Tablets, USP (AF) is 80 mg and is initiated as shown in the dosing algorithm described below. The 80 mg dose can be titrated upward to 100mg or 120mg during initial hospitalization or after discharge on 80 mg in the event of recurrence, by rehospitalization and repeating the same steps used during the initiation of therapy (see Upward Titration of Dose). Patients with atrial fibrillation should be anticoagulated according to usual medical practice. Hypokalemia should be corrected before initiation of sotalol hydrochloride tablet (AF) therapy (see WARNINGS, Ventricular Arrhythmia). Patients to be discharged on sotalol hydrochloride tablet (AF) therapy from an in-patient setting should have an adequate supply of sotalol hydrochloride tablets (AF), to allow uninterrupted therapy until the patient can fill a sotalol hydrochloride tablets (AF) prescription. Initiation of Sotalol Hydrochloride Tablets, USP (AF) TherapyStep 1. Electrocardiographic assessment: Prior to administration of the first dose, the QT interval must be determined using an average of 5 beats. If the baseline QT is greater than 450 msec (JT ≥330 msec if QRS over 100 msec), sotalol hydrochloride tablets (AF) are contraindicated.
Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance should be calculated using the following formula:
creatinine clearance (male) = (140-age)x body weight in kg 72 x serum creatinine (mg/dL) creatinine clearance (female) = (140-age)x body weight in kg x 0.85 72 x serum creatinine (mg/dL)When serum creatinine is given in mcmol/L, divide the value by 88.4 (1 mg/dL= 88.4 mcmol/L).
Step 3. Starting Dose: The starting dose of sotalol hydrochloride tablets (AF) is 80 mg twice daily (BID) if the creatinine clearance is >60 mL/min, and 80 mg once daily (QD) if the creatinine clearance is 40 to 60 mL/min. If the creatinine clearance is <40 mL/min sotalol hydrochloride tablets (AF) are contraindicated.
Step 4. Administer the appropriate daily dose of sotalol hydrochloride tablets (AF) and begin continuous ECG monitoring with QT interval measurements 2 to 4 hours after each dose.
Step 5. If the 80 mg dose level is tolerated and the QT interval remains <500 msec after at least 3 days (after 5 or 6 doses if patient receiving QD dosing), the patient can be discharged. Alternatively, during hospitalization, the dose can be increased to 100 mg or 120 mg BID and the patient followed for 3 days on this dose (followed for 5 or 6 doses if patient receiving QD doses).
The steps described above are summarized in the following diagram:
Place Patient on Telemetry Check Baseline QT If QT >450 msec Sotalol hydrochloride tablets (AF) are CONTRAINDICATED If QT ≤450 msec, proceed Calculate Creatine Clearance (Clcr) If Clcr is <40 mL/min sotalol hydrochloride tablets (AF) are CONTRAINDICATED
If Clcr is 40 to 60 mL/min
start sotalol hydrochloride tablets (AF) 80 mg QD If Clcr is >60 mL/min
start sotalol hydrochloride tablets (AF) 80 mg BID Monitor QT 2 to 4 hours after each dose. If QT ≥500 msec discontinue sotalol hydrochloride tablets (AF). If QT <500 msec after 3 days (after 5th or 6th dose if patient receiving QD dosing) discharge patient on current treatment. Alternatively, during hospitalization, the dose can be increased to 120 mg BID and the patient followed for 3 days on this dose Followed for 5 or 6 doses if patient receiving QD doses).
Upward Titration of DoseIf the 80 mg dose level (given BID or QD depending upon the creatinine clearance) does not reduce the frequency of relapses of AFIB/AFL and is tolerated without excessive QT interval prolongation (i.e., ≥520 msec), the dose level may be increased to 120 mg (BID or QD depending upon the creatinine clearance). As proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment, Steps 2 through 5 used during initiation of sotalol hydrochloride tablet (AF) therapy should be followed when increasing the dose level. In the U.S. multicenter dose-response study, the 120 mg dose (BID or QD) was found to be the most effective in prolonging the time to ECG documented symptomatic recurrence of AFIB/AFL. If the 120 mg dose does not reduce the frequency of early relapse of AFIB/AFL and is tolerated without excessive QT interval prolongation (≥520 msec), an increase to 160 mg (BID or QD depending upon the creatinine clearance), can be considered. Steps 2 through 5 used during the initiation of therapy should be used again to introduce such an increase.
Maintenance of Sotalol Hydrochloride Tablets, USP (AF) TherapyRenal function and QT should be re-evaluated regularly if medically warranted. If QT is 520 msec or greater (JT 430 msec or greater if QRS is >100 msec), the dose of sotalol hydrochloride tablets (AF) therapy should be reduced and patients should be carefully monitored until QT returns to less than 520 msec. If the QT interval is ≥520 msec while on the lowest maintenance dose level (80 mg) the drug should be discontinued. If renal function deteriorates, reduce the daily dose in half by administering the drug once daily as described in Initiation of sotalol hydrochloride tablets (AF) Therapy, Step 3.
Special ConsiderationsThe maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 160 mg BID, doses greater than 160 mg BID have been associated with an increased incidence of Torsade de Pointes and are not recommended.
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
Dosing and Administration in ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater
For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger
For children aged about 2 years or younger the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 x 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 x 0.68)=20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 x 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride tablets (AF) should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
The use of sotalol hydrochloride tablets (AF) in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets (AF) from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride for the maintenance of normal sinus should be transferred to sotalol hydrochloride tablets (AF) because of the significant differences in labeling (i.e., patient package insert, dosing administration, and safety information).
Transfer to Sotalol Hydrochloride Tablets (AF) from Other Antiarrhythmic AgentsBefore starting sotalol hydrochloride tablets (AF), previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see DRUG INTERACTIONS). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets (AF) should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride (AF) syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride (AF) 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for approximately two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol hydrochloride. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol hydrochloride (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity for three (3) months.
-
Lake Erie Medical Dba Quality Care Products Llc
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Lake Erie Medical Dba Quality Care Products Llc
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc] Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
American Health Packaging
![Sotalol Hydrochloride Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | American Health Packaging
![Sotalol Hydrochloride Tablet [American Health Packaging] Sotalol Hydrochloride Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE) and the dosage of sotalol hydrochloride tablets must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 mg/day or 320 mg/day (120 mg to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 mg/day to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 mg/day to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater: For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger: For children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)= 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults, sotalol hydrochloride tablets should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal ImpairmentAdults: Because sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance
Dosing* Interval
mL/min
(hours)
>60
12
30-59
24
10-29
36-48
<10
Dose should be individualized
*The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride tablets has increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above).
Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
Children: The use of sotalol hydrochloride tablets in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride TabletsBefore starting sotalol hydrochloride tablets, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see PRECAUTIONS, Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
1. Measure 120 mL of Simple Syrup. 2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. 3. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. 4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. 5. Allow the tablets to hydrate for at least two hours. 6. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol hydrochloride. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol hydrochloride (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity.
Transfer to Betapace AF from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Lake Erie Medical Dba Quality Care Products Llc
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Lake Erie Medical Dba Quality Care Products Llc
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc] Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Golden State Medical Supply, Inc.
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Golden State Medical Supply, Inc.
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.] Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing and Administration in Adults • Therapy with sotalol hydrochloride tablets (AF) must be initiated (and, if necessary, titrated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of 3 days on the maintenance dose. In addition, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm.
• The QT interval is used to determine patient eligibility for sotalol hydrochloride tablets (AF) treatment and for monitoring safety during treatment. The baseline QT interval must be ≤450 msec in order for a patient to be started on sotalol hydrochloride tablets (AF) therapy. During initiation and titration, the QT interval should be monitored 2 to 4 hours after each dose. If the QT interval prolongs to 500 msec or greater, the dose must be reduced or the drug discontinued.
• The dose of sotalol hydrochloride tablets, USP (AF) must be individualized according to calculated creatinine clearance. In patients with a creatinine clearance >60 mL/min sotalol hydrochloride tablets (AF) are administered twice daily (BID) while in those with a creatinine clearance between 40 and 60 mL/min, the dose is administered once daily (QD) or half the dose is administered twice daily (BID). In patients with a creatinine clearance less than 40 mL/min sotalol hydrochloride tablets (AF) are contraindicated. The recommended initial dose of sotalol hydrochloride tablets (AF) is 80 mg and is initiated as shown in the dosing algorithm described below. The 80 mg dose can be titrated upward to 100 mg or 120 mg during initial hospitalization or after discharge on 80 mg in the event of recurrence, by rehospitalization and repeating the same steps used during the initiation of therapy (see DOSAGE ADMINISTRATION, Upward Titration of Dose).
• Patients with atrial fibrillation should be anticoagulated according to usual medical practice. Hypokalemia should be corrected before initiation of sotalol hydrochloride tablets (AF) therapy (see WARNINGS, Ventricular Arrhythmia).
• Patients to be discharged on sotalol hydrochloride tablets (AF) therapy from an in-patient setting should have an adequate supply of sotalol hydrochloride tablets (AF), to allow uninterrupted therapy until the patient can fill a sotalol hydrochloride tablets (AF) prescription. Initiation of Sotalol Hydrochloride Tablets, USP (AF) TherapyStep 1. Electrocardiographic assessment: Prior to administration of the first dose, the QT interval must be determined using an average of 5 beats. If the baseline QT is greater than 450 msec (JT ≥330 msec if QRS over 100 msec), sotalol hydrochloride tablets (AF) are contraindicated.
Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance should be calculated using the following formula:
creatinine clearance (male) =
(140-age)x body weight in kg
72 x serum creatinine (mg/dL)
creatinine clearance (female) =
(140-age)x body weight in kg x 0.85
72 x serum creatinine (mg/dL)
When serum creatinine is given in μmol/L, divide the value by 88.4 (1 mg/dL = 88.4 μmol/L).
Step 3. Starting Dose: The starting dose of sotalol hydrochloride tablets (AF) is 80 mg twice daily (BID) if the creatinine clearance is >60 mL/min, and 80 mg once daily (QD) if the creatinine clearance is 40-60 mL/min. If the creatinine clearance is <40 mL/min sotalol hydrochloride tablets (AF) are contraindicated.
Step 4. Administer the appropriate daily dose of sotalol hydrochloride tablets (AF) and begin continuous ECG monitoring with QT interval measurements 2 to 4 hours after each dose.
Step 5. In patients with a creatinine clearance >60 mL/min, if the 80 mg dose level is tolerated and the QT interval remains <500 msec after at least 3 days (after 5 or 6 doses if patient receiving QD dosing), the patient can be discharged. Alternatively, during hospitalization, the dose can be increased to 100 mg or 120 mg BID and the patient followed for 3 days on this dose (followed for 5 or 6 doses if patient receiving QD doses).
The steps described above are summarized in the following diagram:
Place Patient on Telemetry
Check Baseline QT
If QT >450 msec sotalol hydrochloride tablets (AF) are CONTRAINDICATED
If QT ≤450 msec, proceed
Calculate Creatine Clearance (Clcr)
If Clcr is <40 mL/min sotalol hydrochloride tablets (AF) are CONTRAINDICATED
If Clcr is 40-60 mL/min start sotalol hydrochloride tablets (AF) 80 mg QD
If Clcr is >60 mL/min start sotalol hydrochloride tablets (AF) 80 mg BID
Monitor QT 2 to 4 hours after each dose.
If QT ≥500 msec discontinue sotalol hydrochloride tablets (AF)
If QT <500 msec after 3 days (after 5th or 6th dose if
patient receiving QD dosing)
discharge patient on current treatment. Alternatively, during
hospitalization, the dose can be increased to 120 mg BID
and the patient followed for 3 days on this dose (followed for 5 or
6 doses if patient receiving QD doses).
Upward Titration of DoseIf the 80 mg dose level (given BID or QD depending upon the creatinine clearance) does not reduce the frequency of relapses of AFIB/AFL and is tolerated without excessive QT interval prolongation (i.e., ≥520 msec), the dose level may be increased to 120 mg (BID or QD depending upon the creatinine clearance). As proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment, Steps 2 through 5 used during initiation of sotalol hydrochloride tablet (AF) therapy should be followed when increasing the dose level. In the U.S. multicenter dose-response study, the 120 mg dose (BID or QD) was found to be the most effective in prolonging the time to ECG documented symptomatic recurrence of AFIB/AFL. If the 120 mg dose does not reduce the frequency of early relapse of AFIB/AFL and is tolerated without excessive QT interval prolongation (≥520 msec), an increase to 160 mg (BID or QD depending upon the creatinine clearance), can be considered. Steps 2 through 5 used during the initiation of therapy should be used again to introduce such an increase.
Maintenance of Sotalol Hydrochloride Tablets, USP (AF) TherapyRenal function and QT should be re-evaluated regularly if medically warranted. If QT is 520 msec or greater (JT 430 msec or greater if QRS is > 100 msec), the dose of sotalol hydrochloride tablets (AF) therapy should be reduced and patients should be carefully monitored until QT returns to less than 520 msec. If the QT interval is ≥520 msec while on the lowest maintenance dose level (80 mg) the drug should be discontinued. If renal function deteriorates, reduce the daily dose in half by administering the drug once daily as described in Initiation of sotalol hydrochloride tablets (AF) therapy, Step 3.
Special ConsiderationsThe maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 160 mg BID, doses greater than 160 mg BID have been associated with an increased incidence of Torsade de Pointes and are not recommended.
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
-
Eon Labs, Inc.
![Sotalol Hydrochloride Tablet [Eon Labs, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Eon Labs, Inc.
![Sotalol Hydrochloride Tablet [Eon Labs, Inc.] Sotalol Hydrochloride Tablet [Eon Labs, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE) and the dosage of sotalol hydrochloride tablets must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 mg/day or 320 mg/day (120 mg to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 mg/day to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 mg/day to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater: For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger: For children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)= 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults, sotalol hydrochloride tablets should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal ImpairmentAdults: Because sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance
Dosing* Interval
mL/min
(hours)
>60
12
30-59
24
10-29
36-48
<10
Dose should be individualized
*The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride tablets has increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above).
Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
Children: The use of sotalol hydrochloride tablets in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride TabletsBefore starting sotalol hydrochloride tablets, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see PRECAUTIONS, Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
1. Measure 120 mL of Simple Syrup. 2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. 3. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. 4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. 5. Allow the tablets to hydrate for at least two hours. 6. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol hydrochloride. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol hydrochloride (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity.
Transfer to Betapace AF from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Teva Pharmaceuticals Usa Inc
![Sotalol Hydrochloride Tablet [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Teva Pharmaceuticals Usa Inc
![Sotalol Hydrochloride Tablet [Teva Pharmaceuticals Usa Inc] Sotalol Hydrochloride Tablet [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol hydrochloride tablets USP, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For Children Aged About 2 Years and GreaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For Children Aged about 2 Years or YoungerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
* The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations. Creatinine Clearance mL/min Dosing* Interval (hours) > 60 12 30 to 59 24 10 to 29 36 to 48 < 10 Dose should be individualizedSince the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets USPBefore starting sotalol hydrochloride tablets USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient’s clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6 ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride tablets USP, 120 mg to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCl. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCl (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature, (15° to 30°C / 59° to 86°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Aidarex Pharmaceuticals Llc
![Sotalol Hydrochloride Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Aidarex Pharmaceuticals Llc
![Sotalol Hydrochloride Tablet [Aidarex Pharmaceuticals Llc] Sotalol Hydrochloride Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets, USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets, USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets, USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets, USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
PediatricsPediatric dosing information for sotalol hydrochloride tablets is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled for pediatric use.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
CreatinineClearance
mL/min
DosingaInterval
(hours)
>60 12 30-59 24 10-29 36-48 <10 Dose should be individualizeda) The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets, USPBefore starting sotalol hydrochloride tablets, USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets, USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionInformation relating to the preparation of an extemporaneous oral solution of sotalol is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled with that information.
Transfer to Betapace AF from Sotalol Hydrochloride Tablets, USPPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets, USP for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Avkare, Inc.
![Sotalol Hydrochloride (Sotalol Hydrochloride) Tablet [Avkare, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Avkare, Inc.
![Sotalol Hydrochloride (Sotalol Hydrochloride) Tablet [Avkare, Inc.] Sotalol Hydrochloride (Sotalol Hydrochloride) Tablet [Avkare, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing and Administration in Adults Therapy with sotalol hydrochloride tablets (AF) must be initiated (and, if necessary, titrated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of 3 days on the maintenance dose. In addition, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm. The QT interval is used to determine patient eligibility for sotalol hydrochloride tablets (AF) treatment and for monitoring safety during treatment. The baseline QT interval must be ≤450 msec in order for a patient to be started on sotalol hydrochloride tablets (AF) therapy. During initiation and titration, the QT interval should be monitored 2 to 4 hours after each dose. If the QT interval prolongs to 500 msec or greater, the dose must be reduced or the drug discontinued. The dose of sotalol hydrochloride tablets, USP (AF) must be individualized according to calculated creatinine clearance. In patients with a creatinine clearance >60 mL/min sotalol hydrochloride tablets (AF) are administered twice daily (BID) while in those with a creatinine clearance between 40 and 60 mL/min, the dose is administered once daily (QD) or half the dose is administered twice daily (BID). In patients with a creatinine clearance less than 40 mL/min sotalol hydrochloride tablets (AF) are contraindicated. The recommended initial dose of sotalol hydrochloride tablets (AF) is 80 mg and is initiated as shown in the dosing algorithm described below. The 80 mg dose can be titrated upward to 100 mg or 120 mg during initial hospitalization or after discharge on 80 mg in the event of recurrence, by rehospitalization and repeating the same steps used during the initiation of therapy (see DOSAGE AND ADMINISTRATION,Upward Titration of Dose). Patients with atrial fibrillation should be anticoagulated according to usual medical practice. Hypokalemia should be corrected before initiation of sotalol hydrochloride tablets (AF) therapy (see WARNINGS, Ventricular Arrhythmia). Patients to be discharged on sotalol hydrochloride tablets (AF) therapy from an in-patient setting should have an adequate supply of sotalol hydrochloride tablets (AF), to allow uninterrupted therapy until the patient can fill a sotalol hydrochloride tablets (AF) prescription. Initiation of Sotalol Hydrochloride Tablets, USP (AF) TherapyStep 1. Electrocardiographic assessment: Prior to administration of the first dose, the QT interval must be determined using an average of 5 beats. If the baseline QT is greater than 450 msec (JT ≥330 msec if QRS over 100 msec), sotalol hydrochloride tablets (AF) are contraindicated.
Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance should be calculated using the following formula:
creatinine clearance (male) = (140-age)x body weight in kg 72 x serum creatinine (mg/dL) creatinine clearance (female) = (140-age)x body weight in kg x 0.85 72 x serum creatinine (mg/dL)When serum creatinine is given in μmol/L, divide the value by 88.4 (1 mg/dL = 88.4 mcmol/L).
Step 3. Starting Dose: The starting dose of sotalol hydrochloride tablets (AF) is 80 mg twice daily (BID) if the creatinine clearance is >60 mL/min, and 80 mg once daily (QD) if the creatinine clearance is 40 to 60 mL/min. If the creatinine clearance is <40 mL/min sotalol hydrochloride tablets (AF) are contraindicated.
Step 4. Administer the appropriate daily dose of sotalol hydrochloride tablets (AF) and begin continuous ECG monitoring with QT interval measurements 2 to 4 hours after each dose.
Step 5. In patients with a creatinine clearance >60 mL/min, if the 80 mg dose level is tolerated and the QT interval remains <500 msec after at least 3 days (after 5 or 6 doses if patient receiving QD dosing), the patient can be discharged. Alternatively, during hospitalization, the dose can be increased to 100 mg or 120 mg BID and the patient followed for 3 days on this dose (followed for 5 or 6 doses if patient receiving QD doses).
The steps described above are summarized in the following diagram:
Place Patient on Telemetry
Check Baseline QT
If QT >450 msec sotalol hydrochloride tablets (AF) are CONTRAINDICATED
If QT ≤450 msec, proceed
Calculate Creatine Clearance (Clcr)
If Clcr is <40 mL/min sotalol hydrochloride tablets (AF) are CONTRAINDICATED
If Clcr is 40-60 mL/min start sotalol hydrochloride tablets (AF) 80 mg QD
If Clcr is >60 mL/min start sotalol hydrochloride tablets (AF) 80 mg BID
Monitor QT 2 to 4 hours after each dose.
If QT ≥500 msec discontinue sotalol hydrochloride tablets (AF)
If QT <500 msec after 3 days (after 5th or 6th dose if
patient receiving QD dosing)
discharge patient on current treatment. Alternatively, during
hospitalization, the dose can be increased to 120 mg BID
and the patient followed for 3 days on this dose (followed for 5 or
6 doses if patient receiving QD doses).
Upward Titration of DoseIf the 80 mg dose level (given BID or QD depending upon the creatinine clearance) does not reduce the frequency of relapses of AFIB/AFL and is tolerated without excessive QT interval prolongation (i.e., ≥520 msec), the dose level may be increased to 120 mg (BID or QD depending upon the creatinine clearance). As proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment, Steps 2 through 5 used during initiation of sotalol hydrochloride tablet (AF) therapy should be followed when increasing the dose level. In the U.S. multicenter dose-response study, the 120 mg dose (BID or QD) was found to be the most effective in prolonging the time to ECG documented symptomatic recurrence of AFIB/AFL. If the 120 mg dose does not reduce the frequency of early relapse of AFIB/AFL and is tolerated without excessive QT interval prolongation (≥520 msec), an increase to 160 mg (BID or QD depending upon the creatinine clearance), can be considered. Steps 2 through 5 used during the initiation of therapy should be used again to introduce such an increase.
Maintenance of Sotalol Hydrochloride Tablets, USP (AF) TherapyRenal function and QT should be re-evaluated regularly if medically warranted. If QT is 520 msec or greater (JT 430 msec or greater if QRS is > 100 msec), the dose of sotalol hydrochloride tablets (AF) therapy should be reduced and patients should be carefully monitored until QT returns to less than 520 msec. If the QT interval is ≥520 msec while on the lowest maintenance dose level (80 mg) the drug should be discontinued. If renal function deteriorates, reduce the daily dose in half by administering the drug once daily as described in Initiation of sotalol hydrochloride tablets (AF) Therapy, Step 3.
Special ConsiderationsThe maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 160 mg BID, doses greater than 160 mg BID have been associated with an increased incidence of Torsade de Pointes and are not recommended.
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
Dosing and Administration in ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater
For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger
For children aged about 2 years or younger the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)=20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride tablets (AF) should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
The use of sotalol hydrochloride tablets (AF) in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets (AF) from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride for the maintenance of normal sinus should be transferred to sotalol hydrochloride tablets (AF) because of the significant differences in labeling (i.e., patient package insert, dosing administration, and safety information).
Transfer to Sotalol Hydrochloride Tablets (AF) from Other Antiarrhythmic AgentsBefore starting sotalol hydrochloride tablets (AF), previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see DRUG INTERACTIONS). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets (AF) should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride (AF) Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride (AF) 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for approximately two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCl. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCl (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable when stored at controlled room temperature (15° to 30°C/59° to 86°F) and ambient humidity for three (3) months.
-
American Health Packaging
![Sotalol Hydrochloride Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | American Health Packaging
![Sotalol Hydrochloride Tablet [American Health Packaging] Sotalol Hydrochloride Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets, USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets, USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets, USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets, USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
PediatricsPediatric dosing information for sotalol hydrochloride tablets is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled for pediatric use.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min
Dosinga
Interval
(hours)
>60
12
30-59
24
10-29
36-48
<10
Dose should be individualized
a) The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets, USPBefore starting sotalol hydrochloride tablets, USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets, USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionInformation relating to the preparation of an extemporaneous oral solution of sotalol is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled with that information.
Transfer to Betapace AF from Sotalol Hydrochloride Tablets, USPPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets, USP for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Mylan Pharmaceuticals Inc.
![Sotalol Hydrochloride Tablet [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Mylan Pharmaceuticals Inc.
![Sotalol Hydrochloride Tablet [Mylan Pharmaceuticals Inc.] Sotalol Hydrochloride Tablet [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing and Administration in Adults • Therapy with sotalol hydrochloride tablets (AF) must be initiated (and, if necessary, titrated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of 3 days on the maintenance dose. In addition, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm. • The QT interval is used to determine patient eligibility for sotalol hydrochloride tablet (AF) treatment and for monitoring safety during treatment. The baseline QT interval must be ≤ 450 msec in order for a patient to be started on sotalol hydrochloride tablet (AF) therapy. During initiation and titration, the QT interval should be monitored 2 to 4 hours after each dose. If the QT interval prolongs to 500 msec or greater, the dose must be reduced or the drug discontinued. • The dose of sotalol hydrochloride tablets (AF) must be individualized according to calculated creatinine clearance. In patients with a creatinine clearance > 60 mL/min sotalol hydrochloride tablets (AF) are administered twice daily (BID) while in those with a creatinine clearance between 40 and 60 mL/min, the dose is administered once daily (QD). In patients with a creatinine clearance less than 40 mL/min sotalol hydrochloride tablets (AF) are contraindicated. The recommended initial dose of sotalol hydrochloride tablets (AF) is 80 mg and is initiated as shown in the dosing algorithm described below. The 80 mg dose can be titrated upward to 120 mg during initial hospitalization or after discharge on 80 mg in the event of recurrence, by rehospitalization and repeating the same steps used during the initiation of therapy (see DOSAGE AND ADMINISTRATION: Upward Titration of Dose). • Patients with atrial fibrillation should be anticoagulated according to usual medical practice. Hypokalemia should be corrected before initiation of sotalol hydrochloride tablet (AF) therapy (see WARNINGS: Ventricular Arrhythmia). • Patients to be discharged on sotalol hydrochloride tablet (AF) therapy from an in-patient setting should have an adequate supply of sotalol hydrochloride tablets (AF), to allow uninterrupted therapy until the patient can fill a sotalol hydrochloride tablets (AF) prescription. Initiation of Sotalol Hydrochloride Tablet (AF) TherapyStep 1. Electrocardiographic assessment: Prior to administration of the first dose, the QT interval must be determined using an average of five beats. If the baseline QT is greater than 450 msec (JT ≥ 330 msec if QRS over 100 msec), sotalol hydrochloride tablets (AF) are contraindicated.
Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance should be calculated using the following formula:
creatinine clearance (male) =
(140-age) × body weight in kg
72 × serum creatinine (mg/dL)
creatinine clearance (female) =
(140-age) × body weight in kg × 0.85
72 × serum creatinine (mg/dL)
When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L).
Step 3. Starting Dose: The starting dose of sotalol hydrochloride tablets (AF) is 80 mg twice daily (BID) if the creatinine clearance is > 60 mL/min, and 80 mg once daily (QD) if the creatinine clearance is 40 to 60 mL/min. If the creatinine clearance is < 40 mL/min sotalol hydrochloride tablets (AF) are contraindicated.
Step 4. Administer the appropriate daily dose of sotalol hydrochloride tablets (AF) and begin continuous ECG monitoring with QT interval measurements 2 to 4 hours after each dose.
Step 5. If the 80 mg dose level is tolerated and the QT interval remains < 500 msec after at least 3 days (after 5 or 6 doses if patient receiving QD dosing), the patient can be discharged. Alternatively, during hospitalization, the dose can be increased to 120 mg BID and the patient followed for 3 days on this dose (followed for 5 or 6 doses if patient receiving QD doses).
The steps described above are summarized in the following diagram:
Upward Titration of DoseIf the 80 mg dose level (given BID or QD depending upon the creatinine clearance) does not reduce the frequency of relapses of AFIB/AFL and is tolerated without excessive QT interval prolongation (i.e., ≥ 520 msec), the dose level may be increased to 120 mg (BID or QD depending upon the creatinine clearance). As proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment, Steps 2 through 5 used during initiation of sotalol hydrochloride tablets (AF) therapy should be followed when increasing the dose level. In the U.S. multicenter dose-response study, the 120 mg dose (BID or QD) was found to be the most effective in prolonging the time to ECG documented symptomatic recurrence of AFIB/AFL. If the 120 mg dose does not reduce the frequency of early relapse of AFIB/AFL and is tolerated without excessive QT interval prolongation (≥ 520 msec), an increase to 160 mg (BID or QD depending upon the creatinine clearance), can be considered. Steps 2 through 5 used during the initiation of therapy should be used again to introduce such an increase.
Maintenance of Sotalol Hydrochloride Tablet (AF) TherapyRenal function and QT should be reevaluated regularly if medically warranted. If QT is 520 msec or greater (JT 430 msec or greater if QRS is > 100 msec), the dose of sotalol hydrochloride tablet (AF) therapy should be reduced and patients should be carefully monitored until QT returns to less than 520 msec. If the QT interval is ≥ 520 msec while on the lowest maintenance dose level (80 mg) the drug should be discontinued. If renal function deteriorates, reduce the daily dose in half by administering the drug once daily as described in Initiation of Sotalol Hydrochloride Tablet (AF) Therapy, Step 3.
Special ConsiderationsThe maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 160 mg BID, doses greater than 160 mg BID have been associated with an increased incidence of Torsades de pointes and are not recommended.
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
Dosing and Administration in ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For Children Aged About 2 Years and GreaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For Children Aged About 2 Years or YoungerFor children aged about 2 years or younger the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 × 0.97) = 29.1 mg/m2, administered 3 times daily. For a child aged one month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 × 0.68) = 20 mg/m2, administered 3 times daily. For a child aged about one week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 × 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride tablets (AF) should be used with particular caution in children if the QTc is greater than 500 msec on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
The use of sotalol hydrochloride tablets (AF) in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol hydrochloride tablets (AF) in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets (AF) from Sotalol Hydrochloride TabletsPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets for the maintenance of normal sinus should be transferred to sotalol hydrochloride tablets (AF) because of the significant differences in labeling (i.e., patient package insert, dosing administration, and safety information).
Transfer to Sotalol Hydrochloride Tablets (AF) from Other Antiarrhythmic AgentsBefore starting sotalol hydrochloride tablets (AF), previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see PRECAUTIONS: Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets (AF) should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol Hydrochloride (AF) Syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
1. Measure 120 mL of Simple Syrup. 2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. 3. Add five (5) sotalol hydrochloride (AF) 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. 4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. 5. Allow the tablets to hydrate for approximately 2 hours. 6. After at least 2 hours have elapsed, shake the bottle intermittently over the course of at least another 2 hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol hydrochloride. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol hydrochloride (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable when stored at 20° to 25°C/68° to 77°F [see USP Controlled Room Temperature] and ambient humidity for three (3) months.
-
Bryant Ranch Prepack
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Bryant Ranch Prepack
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack] Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Carilion Materials Management
![Sotalol Hydrochloride Tablet [Carilion Materials Management]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Carilion Materials Management
![Sotalol Hydrochloride Tablet [Carilion Materials Management] Sotalol Hydrochloride Tablet [Carilion Materials Management]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see ). Sotalol should be administered only after appropriate clinical assessment (see ), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment. INDICATIONS AND USAGEINDICATIONS AND USAGE
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QT interval and heart rate. c
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see ) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended. CLINICAL PHARMACOLOGY
For initiation of treatment, 30 mg/m three times a day (90 mg/m total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QT , with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function. 222c
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m , administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m , administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m . Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer. 222
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QT is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QT exceeds 550 msec. cc
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance mL/min
Dosing Interval (hours) a
>60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations. a
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QT is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration. c
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see ). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see ). Drug InteractionsWARNINGS
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF from Sotalol ®Patients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF , dosing administration, and safety information). ®®
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QT interval and heart rate. c
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see ) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended. CLINICAL PHARMACOLOGY
For initiation of treatment, 30 mg/m three times a day (90 mg/m total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QT , with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function. 222c
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m , administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m , administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m . Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer. 222
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QT is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QT exceeds 550 msec. cc
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see ) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended. CLINICAL PHARMACOLOGY
For initiation of treatment, 30 mg/m three times a day (90 mg/m total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QT , with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function. 222c
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m , administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m , administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m . Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer. 222
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QT is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QT exceeds 550 msec. cc
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance mL/min
Dosing Interval (hours) a
>60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations. a
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QT is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration. c
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine Clearance mL/min
Dosing Interval (hours) a
>60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations. a
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QT is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration. c
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see ). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see ). Drug InteractionsWARNINGS
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF from Sotalol ®Patients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF , dosing administration, and safety information). ®®
-
Bryant Ranch Prepack
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Bryant Ranch Prepack
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack] Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
AdultsDosage of sotalol hydrochloride should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
ChildrenAs in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
For children aged about 2 years and greaterFor children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children (see CLINICAL PHARMACOLOGY) is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended.
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or youngerFor children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97) = 29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68) = 20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol hydrochloride should be used with particular caution in children if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 msec.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
Creatinine
Clearance
mL/min Dosinga
Interval
(hours) >60 12 30 to 59 24 10 to 29 36 to 48 <10 Dose should be individualizedaThe initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol hydrochloride in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to SotalolBefore starting sotalol, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionSotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) available from Humco Laboratories as follows:
Measure 120 mL of Simple Syrup. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. NOTE: An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. NOTE: The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved. Allow the tablets to hydrate for at least two hours. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. NOTE: The tablets can be allowed to hydrate overnight to simplify the disintegration process.The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol HCI. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
This extemporaneously prepared oral solution of sotalol HCI (with suspended inactive particles) must be shaken well prior to administration. This is to ensure that the amount of inactive solid particles per dose remains constant throughout the duration of use.
Stability studies indicate that the suspension is stable for three months when stored at controlled room temperature (20°-25°C/68°-77°F) and ambient humidity.
Transfer to Betapace AF® from SotalolPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol for the maintenance of normal sinus rhythm should be transferred to Betapace AF® because of the significant differences in labeling (i.e., patient package insert for Betapace AF®, dosing administration, and safety information).
-
Mylan Institutional Llc
![Sotalol Hydrochloride Injection [Mylan Institutional Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Mylan Institutional Llc
![Sotalol Hydrochloride Injection [Mylan Institutional Llc] Sotalol Hydrochloride Injection [Mylan Institutional Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Rules and Safety Measures of Intravenous Sotalol TherapyFor the safety of the patient, the safety measures required of oral sotalol administration must also be applied for intravenous route. To minimize the risk of induced arrhythmia, patients initiated or re-initiated on sotalol should be hospitalized for at least three days or until steady state drug levels are achieved, in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring. Initiate intravenous sotalol therapy in the presence of personnel trained in the management of serious ventricular arrhythmias. Perform a baseline ECG to determine the QT interval and measure and normalize serum potassium and magnesium levels before initiating therapy with starting sotalol injection. Measure serum creatinine and calculate an estimated creatinine clearance in order to establish the appropriate dosing interval for sotalol.
If the baseline QT is greater than 450 ms (JT >330 ms if QRS over 100 ms), sotalol is not recommended.
The patient's creatinine clearance should be calculated using the one of several formulas. The Cockcroft-Gault formula to determine creatinine clearance is:
Creatinine clearance (male) =
(140-age) × body weight in kg
72 × serum creatinine (mg/dL)
Creatinine clearance (female) =
(140-age) × body weight in kg ×0.85
72 × serum creatinine (mg/dL)
When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L).
Start sotalol therapy only if the baseline QT interval is <450 ms. During initiation and titration, monitor the QT interval after the completion of each infusion If the QT interval prolongs to 500 ms or greater, reduce the dose, decrease the infusion rate, or discontinue the drug.
Administer sotalol twice daily in patients with a creatinine clearance >60 mL/min or once daily) in patients with a creatinine clearance between 40 and 60 mL/min. Sotalol is not recommended in patients with a creatinine clearance <40 mL/min. The recommended initial IV dose of sotalol is 75 mg (once or twice daily) and is initiated as shown in the dosing algorithm described below. The 75 mg dose can be titrated upward to 112.5 or 150 mg after at least 3 days [see Dosage and Administration (2.5)].
2.2 Dose of Intravenous SotalolThe bioavailability of oral sotalol is between 90% and 100%. The corresponding dose of intravenous sotalol is, therefore, slightly less than that of the oral dose. The effects of the initial intravenous dose must be monitored and the dose titrated either upward or downward, if needed, based on clinical effect, QT interval, or adverse reactions.
Table 1: Conversion from Oral Sotalol to Intravenous Sotalol Oral dose
Once or twice daily Intravenous dose
Once or twice daily
Administered over 5 hours80 mg
75 mg (5 mL sotalol injection)
120 mg
112.5 mg (7.5 mL sotalol injection)
160 mg
150 mg (10 mL sotalol injection)
2.3 Preparation of Sotalol InfusionIntravenous sotalol must be diluted for infusion. Appropriate diluents are saline, 5% dextrose in water (D5W), or Ringer's lactate. Usually, prepare in a volume of 100-250 mL. Use a volumetric infusion pump to infuse intravenous sotalol at a constant rate. The following table compensates for dead space in the infusion set.
Table 2: Sotalol Infusion Preparation to Compensate for Dead Space in Infusion Set Target
Dose Sotalol Injection Diluent Volume
Prepared Volume
to Infuse75 mg
6 mL
114 mL
120 mL
100 mL
112.5 mg
9 mL
111 mL
100 mL
150 mg
12 mL
108 mL
100 mL
75 mg
6 mL
294 mL
300 mL
250 mL
112.5 mg
9 mL
291 mL
250 mL
150 mg
12 mL
288 mL
250 mL
2.4 Initiation of Intravenous Sotalol TherapyThe starting dose of intravenous sotalol is 75 mg infused over 5 hours once or twice daily based on the creatinine clearance. Monitor ECG for excessive increase in QTc.
2.5 Upward Titration of DoseIf the 75 mg dose of intravenous sotalol does not reduce the frequency of relapses of life threatening ventricular arrhythmias or symptomatic AFIB/AFL and is tolerated without excessive (i.e., to >500 ms) QTc prolongation, increase the dose to 112.5 mg infused over 5 hours, once or twice daily depending upon the creatinine clearance. Continue to monitor QTc during dose escalations.
2.6 Dose for Ventricular ArrhythmiasThe recommended initial dose of intravenous sotalol is 75 mg infused over 5 hours, once or twice daily based on creatinine clearance. The dose may be increased in increments of 75 mg/day every 3 days. The usual therapeutic effect is observed with oral doses of 80 to 160 mg once or twice a day (corresponding to 75 to 150 mg intravenous sotalol). Oral doses as high as 240-320 mg once or twice a day (corresponding to 225 to 300 mg intravenous sotalol) have been utilized in patients with refractory life-threatening arrhythmias.
2.7 Dose for Symptomatic AFIB/AFLIn the U.S. multicenter dose-response study, 120 mg orally once or twice a day (corresponding to 112.5 mg intravenous sotalol) was found to be the most effective dose in prolonging the time to ECG-documented symptomatic recurrence of AFIB/AFL. If that dose level, at steady state, does not reduce the frequency of early relapse of arrhythmia and is tolerated without excessive QTc prolongation (>520 ms), increase the dose to 160 mg orally once or twice a day (corresponding to 150 mg intravenous sotalol).
2.8 Dosing and Administration in ChildrenIntravenous sotalol has not been studied in children. As in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate.
For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children [see Clinical Pharmacology (12.2)] is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended. For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total oral daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children about 2 years or younger the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph which shows age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 × 0.97) = 29.1 mg/m2, administered orally three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 × 0.68) = 20 mg/m2, administered orally three times daily. For a child aged 1 week, the initial starting oral dose should be multiplied by 0.3; the starting dose would be (30 × 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol should be used with particular caution in children if the QTc is greater than 500 ms on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 ms.
The use of oral sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is most important. It will take much longer to reach steady-state with any dose and/or frequency of administration in these children.
-
Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs] Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
As with other antiarrhythmic agents, sotalol hydrochloride tablets, USP should be initiated and doses increased in a hospital with facilities for cardiac rhythm monitoring and assessment (see INDICATIONS AND USAGE). Sotalol hydrochloride tablets, USP should be administered only after appropriate clinical assessment (see INDICATIONS AND USAGE), and the dosage of sotalol hydrochloride tablets, USP must be individualized for each patient on the basis of therapeutic response and tolerance. Proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment.
AdultsDosage of sotalol hydrochloride tablets, USP should be adjusted gradually, allowing 3 days between dosing increments in order to attain steady-state plasma concentrations, and to allow monitoring of QT intervals. Graded dose adjustment will help prevent the usage of doses which are higher than necessary to control the arrhythmia. The recommended initial dose is 80 mg twice daily. This dose may be increased, if necessary, after appropriate evaluation to 240 or 320 mg/day (120 to 160 mg twice daily). In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses. Some patients with life-threatening refractory ventricular arrhythmias may require doses as high as 480 to 640 mg/day; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events, in particular proarrhythmia. Because of the long terminal elimination half-life of sotalol, dosing on more than a BID regimen is usually not necessary.
PediatricsPediatric dosing information for sotalol hydrochloride tablets is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled for pediatric use.
Dosage in Renal Impairment AdultsBecause sotalol is excreted predominantly in urine and its terminal elimination half-life is prolonged in conditions of renal impairment, the dosing interval (time between divided doses) of sotalol should be modified (when creatinine clearance is lower than 60 mL/min) according to the following table.
CreatinineClearance
mL/min
DosingaInterval
(hours)
>60 12 30-59 24 10-29 36-48 <10 Dose should be individualizeda) The initial dose of 80 mg and subsequent doses should be administered at these intervals. See following paragraph for dosage escalations.
Since the terminal elimination half-life of sotalol hydrochloride is increased in patients with renal impairment, a longer duration of dosing is required to reach steady-state. Dose escalations in renal impairment should be done after administration of at least 5 to 6 doses at appropriate intervals (see table above). Extreme caution should be exercised in the use of sotalol in patients with renal failure undergoing hemodialysis. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Sotalol, however, can be partly removed by dialysis with subsequent partial rebound in concentrations when dialysis is completed. Both safety (heart rate, QT interval) and efficacy (arrhythmia control) must be closely monitored.
ChildrenThe use of sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is more important and it will take much longer to reach steady-state with any dose and/or frequency of administration.
Transfer to Sotalol Hydrochloride Tablets, USPBefore starting sotalol hydrochloride tablets, USP, previous antiarrhythmic therapy should generally be withdrawn under careful monitoring for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits (see Drug Interactions). Treatment has been initiated in some patients receiving I.V. lidocaine without ill effect. After discontinuation of amiodarone, sotalol hydrochloride tablets, USP should not be initiated until the QT interval is normalized (see WARNINGS).
Preparation of Extemporaneous Oral SolutionInformation relating to the preparation of an extemporaneous oral solution of sotalol is approved for Berlex Laboratories’ sotalol hydrochloride tablets. However, due to Berlex’s marketing exclusivity rights, this drug product is not labeled with that information.
Transfer to Betapace AF from Sotalol Hydrochloride Tablets, USPPatients with a history of symptomatic AFIB/AFL who are currently receiving sotalol hydrochloride tablets, USP for the maintenance of normal sinus rhythm should be transferred to Betapace AF because of the significant differences in labeling (i.e., patient package insert for Betapace AF, dosing administration, and safety information).
-
Altathera Pharmaceuticals, Llc
![Sotalol Hydrochloride Injection [Altathera Pharmaceuticals, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sotalol Hydrochloride | Altathera Pharmaceuticals, Llc
![Sotalol Hydrochloride Injection [Altathera Pharmaceuticals, Llc] Sotalol Hydrochloride Injection [Altathera Pharmaceuticals, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Rules and Safety Measures of Intravenous Sotalol TherapyFor the safety of the patient, the safety measures required of oral sotalol administration must also be applied for intravenous route. To minimize the risk of induced arrhythmia, patients initiated or re-initiated on sotalol should be hospitalized for at least three days or until steady state drug levels are achieved, in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring. Initiate intravenous sotalol therapy in the presence of personnel trained in the management of serious ventricular arrhythmias. Perform a baseline ECG to determine the QT interval and measure and normalize serum potassium and magnesium levels before initiating therapy with starting sotalol injection. Measure serum creatinine and calculate an estimated creatinine clearance in order to establish the appropriate dosing interval for sotalol.
If the baseline QT is greater than 450 ms (JT >330 ms if QRS over 100 ms), sotalol is not recommended. The patient's creatinine clearance should be calculated using the one of several formulas. The Cockcroft-Gault formula to determine creatinine clearance is:
When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L).
Start sotalol therapy only if the baseline QT interval is <450 ms. During initiation and titration, monitor the QT interval after the completion of each infusion. If the QT interval prolongs to 500 ms or greater, reduce the dose, decrease the infusion rate, or discontinue the drug.
Administer sotalol twice daily in patients with a creatinine clearance >60 mL/min or once daily) in patients with a creatinine clearance between 40 and 60 mL/min. Sotalol is not recommended in patients with a creatinine clearance <40 mL/min. The recommended initial IV dose of sotalol is 75 mg (once or twice daily) and is initiated as shown in the dosing algorithm described below. The 75 mg dose can be titrated upward to 112.5 or 150 mg after at least 3 days [see Dosage and Administration (2.5)].
2.2 Dose of Intravenous SotalolThe bioavailability of oral sotalol is between 90% and 100%. The corresponding dose of intravenous sotalol is, therefore, slightly less than that of the oral dose. The effects of the initial intravenous dose must be monitored and the dose titrated either upward or downward, if needed, based on clinical effect, QT interval, or adverse reactions.
Table 1: Conversion from Oral Sotalol to Intravenous Sotalol Oral dose
Once or twice
daily Intravenous dose
Once or twice
daily
Administered over 5 hours 80 mg 75 mg (5 mL sotalol injection) 120 mg 112.5 mg (7.5 mL sotalol injection) 160 mg 150 mg (10 mL sotalol injection) 2.3 Preparation of Sotalol InfusionIntravenous sotalol must be diluted for infusion. Appropriate diluents are saline, 5% dextrose in water (D5W), or Ringer's lactate. Usually, prepare in a volume of 100-250 mL. Use a volumetric infusion pump to infuse intravenous sotalol at a constant rate. The following table compensates for dead space in the infusion set.
Table 2: Sotalol Infusion Preparation to Compensate for Dead Space in Infusion Set Target
Dose Sotalol Injection Diluent Volume Prepared Volume to Infuse 75 mg 6 mL 114 mL
120 mL 100 mL 112.5 mg 9 mL 111 mL 100 mL 150 mg 12 mL 108 mL 100 mL 75 mg 6 mL 294 mL
300 mL 250 mL 112.5 mg 9 mL 291 mL 250 mL 150 mg 12 mL 288 mL 250 mL 2.4 Initiation of Intravenous Sotalol TherapyThe starting dose of intravenous sotalol is 75 mg infused over 5 hours once or twice daily based on the creatinine clearance. Monitor ECG for excessive increase in QTc.
2.5 Upward Titration of DoseIf the 75 mg dose of intravenous sotalol does not reduce the frequency of relapses of life threatening ventricular arrhythmias or symptomatic AFIB/AFL and is tolerated without excessive (i.e., to >500 ms) QTc prolongation, increase the dose to 112.5 mg infused over 5 hours, once or twice daily depending upon the creatinine clearance. Continue to monitor QTc during dose escalations.
2.6 Dose for Ventricular ArrhythmiasThe recommended initial dose of intravenous sotalol is 75 mg infused over 5 hours, once or twice daily based on creatinine clearance. The dose may be increased in increments of 75 mg/day every 3 days. The usual therapeutic effect is observed with oral doses of 80 to 160 mg once or twice a day (corresponding to 75 to 150 mg intravenous sotalol). Oral doses as high as 240-320 mg once or twice a day (corresponding to 225 to 300 mg intravenous sotalol) have been utilized in patients with refractory life-threatening arrhythmias.
2.7 Dose for Symptomatic AFIB/AFLIn the U.S. multicenter dose-response study, 120 mg orally once or twice a day (corresponding to 112.5 mg intravenous sotalol) was found to be the most effective dose in prolonging the time to ECG- documented symptomatic recurrence of AFIB/AFL. If that dose level, at steady state, does not reduce the frequency of early relapse of arrhythmia and is tolerated without excessive QTc prolongation (>520 ms), increase the dose to 160 mg orally once or twice a day (corresponding to 150 mg intravenous sotalol).
2.8 Dosing and Administration in ChildrenIntravenous sotalol has not been studied in children. As in adults the following precautionary measures should be considered when initiating sotalol treatment in children: initiation of treatment in the hospital after appropriate clinical assessment; individualized regimen as appropriate; gradual increase of doses if required; careful assessment of therapeutic response and tolerability; and frequent monitoring of the QTc interval and heart rate. For children aged about 2 years and greater, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children [see Clinical Pharmacology (12.2)] is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide. From pediatric pharmacokinetic data the following is recommended. For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total oral daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children about 2 years or younger the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph which shows age plotted on a logarithmic scale in months.
For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 × 0.97) = 29.1 mg/m2, administered orally three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 × 0.68) = 20 mg/m2, administered orally three times daily. For a child aged 1 week, the initial starting oral dose should be multiplied by 0.3; the starting dose would be (30 × 0.3) = 9 mg/m2. Similar calculations should be made for increased doses as titration proceeds. Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
In all children, individualization of dosage is required. As in adults sotalol should be used with particular caution in children if the QTc is greater than 500 ms on therapy and serious consideration should be given to reducing the dose or discontinuing therapy when QTc exceeds 550 ms.
The use of oral sotalol in children with renal impairment has not been investigated. Sotalol elimination is predominantly via the kidney in the unchanged form. Use of sotalol in any age group with decreased renal function should be at lower doses or at increased intervals between doses. Monitoring of heart rate and QTc is most important. It will take much longer to reach steady-state with any dose and/or frequency of administration in these children.
Login To Your Free Account

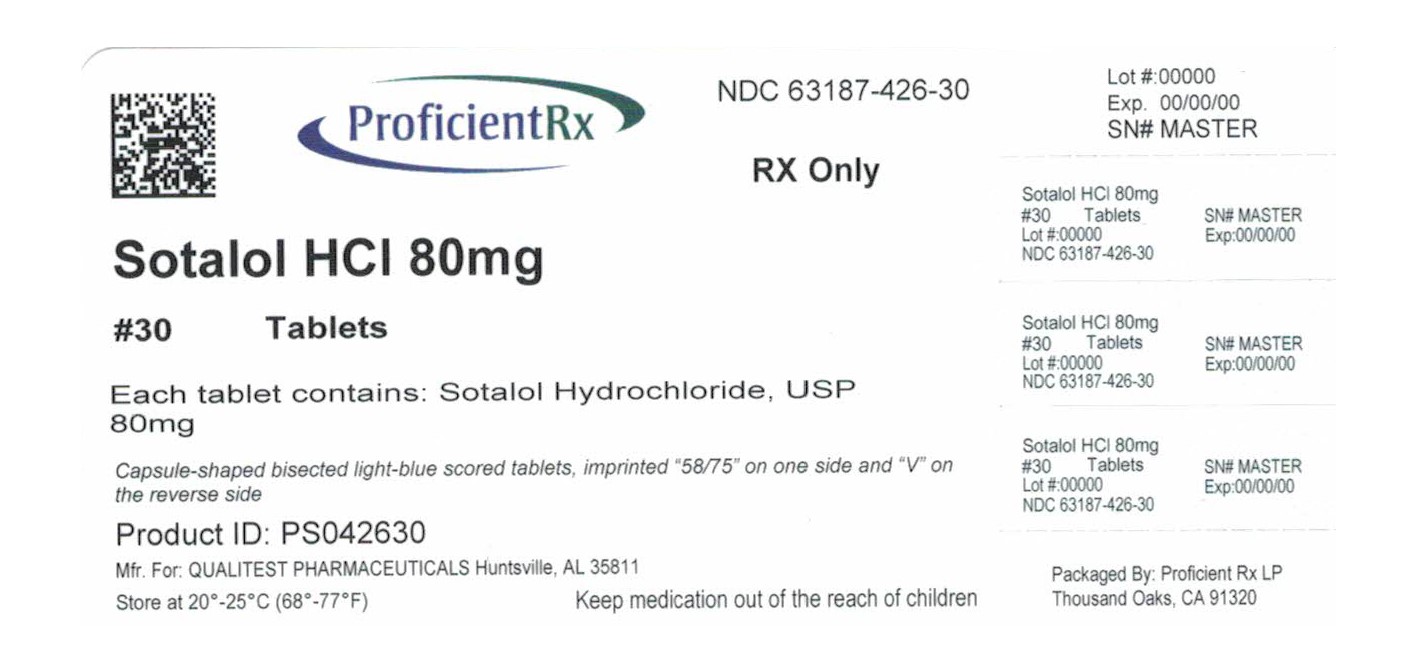

![Sotalol Hydrochloride Tablet [Global Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=f0ee7f5c-3e8b-4104-a95c-5420ebd4092b&name=sotalol-02.jpg)
![Sotalol Hydrochloride Tablet [Rebel Distributors Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6383dc39-15a9-4260-8064-18a8c83004b1&name=6383dc39-15a9-4260-8064-18a8c83004b1-03.jpg)
![Sotalol Hydrochloride Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=dceafc93-2edb-4be7-bbde-014e7778b087&name=43063133.jpg)
![Sotalol Hydrochloride Tablet [Qualitest Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=576905b7-6e6d-4aa0-b690-24be26e70cd2&name=sotalol-3.jpg)
![Sotalol Hydrochloride Tablet [Apotex Corp.]](http://www.recallguide.org/wp-content/themes/recallguide/assets/img/drug-image-placeholder.jpg)
![Sotalol Hydrochloride Tablet [Physicians Total Care, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=1436950d-a07f-43bb-811f-201f2991dbf6&name=4435.jpg)
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6674d53a-7137-4822-8841-4982f702a1b8&name=6674d53a-7137-4822-8841-4982f702a1b8-02.jpg)
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2d1e7246-eb9f-468a-8f52-0c9feae947b3&name=sotalol-hydrochloride-tablets-3.jpg)
![Sotalol Hydrochloride Tablet [Apotex Corp.]](http://www.recallguide.org/wp-content/themes/bootstrap/assets/img/drug-image-placeholder.jpg)
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=7cc5592d-42ca-46b6-99c4-3027bc62f12a&name=SotalolHCl160mgQualitest.jpg)
![Sotalol Hydrochloride Tablet [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a04796d9-0e24-4abd-9f6b-8b9b756b8fd7&name=9db6a76f-6745-4f26-8fb3-cbf6743a360c-03.jpg)
![Sotalol Hydrochloride Tablet [Lake Erie Medical Dba Quality Care Products Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a014b73b-95a5-4ad4-a494-278822db95b9&name=SotalolHCL80mgQualitest.jpg)
![Sotalol Hydrochloride Tablet [Golden State Medical Supply, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=981c90c0-3afd-4fb4-9440-c383df76d4a2&name=56d4a4ad-fbfc-4098-9a7d-1348a250b212-05.jpg)
![Sotalol Hydrochloride Tablet [Eon Labs, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=84562767-c0b0-4a59-a2ed-ea3874176af5&name=401b80f7-8916-4421-be5f-e0647f553c88-03.jpg)
![Sotalol Hydrochloride Tablet [Teva Pharmaceuticals Usa Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=8e2772cb-7dea-42d1-ba31-d479ba7cb09a&name=ec507bf2-ef5d-4d2a-89fa-0a91e6320a07-03.jpg)
![Sotalol Hydrochloride Tablet [Aidarex Pharmaceuticals Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6481858a-353e-4b2a-af48-6c5d13ee0b2a&name=sotalol-80-mg-for-apotex-2.jpg)
![Sotalol Hydrochloride (Sotalol Hydrochloride) Tablet [Avkare, Inc.]](http://recallguide.cwdevelopsp.com/wp-content/themes/recallguide/assets/img/drug-image-placeholder.jpg)
![Sotalol Hydrochloride Tablet [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=4614480b-b36e-4dbd-9fc0-d083890d297d&name=4614480b-b36e-4dbd-9fc0-d083890d297d-02.jpg)
![Sotalol Hydrochloride Tablet [Mylan Pharmaceuticals Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6524fdc2-f931-463d-ba77-b6ab1688fe45&name=321f21be-32d1-49e0-ac9b-813e2547d2ee-06.jpg)
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=86e6e910-5910-4e0a-828c-7eddda12fd94&name=47191.jpg)
![Sotalol Hydrochloride Tablet [Carilion Materials Management]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d288de0a-913d-4617-aa47-c6201ebf2a0d&name=68151-2702.jpg)
![Sotalol Hydrochloride Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3433ddec-0a48-45fc-9850-c9a53147333c&name=47201.jpg)
![Sotalol Hydrochloride Injection [Mylan Institutional Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2afe7385-2441-4e22-b63e-ab8614b275df&name=1a9b03b5-4401-4e83-bfef-53ba0434e846-05.jpg)
![Sotalol Hydrochloride Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5be593e4-72a2-497f-a7ec-b309d4a35629&name=sotalol-hcl-80mg-apotex-2.jpg)
![Sotalol Hydrochloride Injection [Altathera Pharmaceuticals, Llc]](https://www.recallguide.org/wp-content/themes/bootstrap/assets/img/drug-image-placeholder.jpg)