FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Tikosyn Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
TIKOSYN (dofetilide) can cause serious ventricular arrhythmias, primarily Torsade de Pointes (TdP) type ventricular tachycardia, a polymorphic ventricular tachycardia associated with QT interval prolongation. QT interval prolongation is directly related to dofetilide plasma concentration. Factors such as reduced creatinine clearance or certain dofetilide drug interactions will increase dofetilide plasma concentration. The risk of TdP can be reduced by controlling the plasma concentration through adjustment of the initial dofetilide dose according to creatinine clearance and by monitoring the ECG for excessive increases in the QT interval.
Treatment with dofetilide must therefore be started only in patients placed for a minimum of three days in a facility that can provide electrocardiographic monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Calculation of the creatinine clearance for all patients must precede administration of the first dose of dofetilide. For detailed instructions regarding dose selection, see DOSAGE AND ADMINISTRATION.
The risk of dofetilide induced ventricular arrhythmia was assessed in three ways in clinical studies: 1) by description of the QT interval and its relation to the dose and plasma concentration of dofetilide; 2) by observing the frequency of TdP in TIKOSYN-treated patients according to dose; 3) by observing the overall mortality rate in patients with atrial fibrillation and in patients with structural heart disease.
The QT interval increases linearly with increasing TIKOSYN dose (see Figures 1 and 2 in CLINICAL PHARMACOLOGY and Dose-Response and Concentration Response for Increase in QT Interval).
In the supraventricular arrhythmia population (patients with AF and other supraventricular arrhythmias), the overall incidence of Torsade de Pointes was 0.8%. The frequency of TdP by dose is shown in Table 4. There were no cases of TdP on placebo.
| TIKOSYN Dose | |||||
|---|---|---|---|---|---|
| <250 mcg BID | 250 mcg BID | >250–500 mcg BID | >500 mcg BID | All Doses | |
| Number of Patients | 217 | 388 | 703 | 38 | 1346 |
| Torsade de Pointes | 0 | 1 (0.3%) | 6 (0.9%) | 4 (10.5%) | 11 (0.8%) |
As shown in Table 5, the rate of TdP was reduced when patients were dosed according to their renal function (see CLINICAL PHARMACOLOGY, Pharmacokinetics in Special Populations, Renal Impairment and DOSAGE AND ADMINISTRATION).
| Total | Before | After | |
|---|---|---|---|
| Population: | n/N % | n/N % | n/N % |
| Supraventricular Arrhythmias | 11/1346 (0.8%) | 6/193 (3.1%) | 5/1153 (0.4%) |
| DIAMOND CHF | 25/762 (3.3%) | 7/148 (4.7%) | 18/614 (2.9%) |
| DIAMOND MI | 7/749 (0.9%) | 3/101 (3.0%) | 4/648 (0.6%) |
| DIAMOND AF | 4/249 (1.6%) | 0/43 (0%) | 4/206 (1.9%) |
The majority of the episodes of TdP occurred within the first three days of TIKOSYN therapy (10/11 events in the studies of patients with supraventricular arrhythmias; 19/25 and 4/7 events in DIAMOND CHF and DIAMOND MI, respectively; 2/4 events in the DIAMOND AF subpopulation).
In a pooled survival analysis of patients in the supraventricular arrhythmia population (low prevalence of structural heart disease), deaths occurred in 0.9% (12/1346) of patients receiving TIKOSYN and 0.4% (3/677) in the placebo group. Adjusted for duration of therapy, primary diagnosis, age, gender, and prevalence of structural heart disease, the point estimate of the hazard ratio for the pooled studies (TIKOSYN/placebo) was 1.1 (95% CI: 0.3, 4.3). The DIAMOND CHF and MI trials examined mortality in patients with structural heart disease (ejection fraction ≤35%). In these large, double-blind studies, deaths occurred in 36% (541/1511) of TIKOSYN patients and 37% (560/1517) of placebo patients. In an analysis of 506 DIAMOND patients with atrial fibrillation/flutter at baseline, one year mortality on TIKOSYN was 31% vs. 32% on placebo (see CLINICAL STUDIES).
Because of the small number of events, an excess mortality due to TIKOSYN cannot be ruled out with confidence in the pooled survival analysis of placebo-controlled trials in patients with supraventricular arrhythmias. However, it is reassuring that in two large placebo-controlled mortality studies in patients with significant heart disease (DIAMOND CHF/MI), there were no more deaths in TIKOSYN-treated patients than in patients given placebo (see CLINICAL STUDIES).
(see CONTRAINDICATIONS)
Because there is a linear relationship between dofetilide plasma concentration and QTc, concomitant drugs that interfere with the metabolism or renal elimination of dofetilide may increase the risk of arrhythmia (Torsade de Pointes). TIKOSYN is metabolized to a small degree by the CYP3A4 isoenzyme of the cytochrome P450 system and an inhibitor of this system could increase systemic dofetilide exposure. More important, dofetilide is eliminated by cationic renal secretion, and three inhibitors of this process have been shown to increase systemic dofetilide exposure. The magnitude of the effect on renal elimination by cimetidine, trimethoprim, and ketoconazole (all contraindicated concomitant uses with dofetilide) suggests that all renal cation transport inhibitors should be contraindicated.
Hypokalemia or hypomagnesemia may occur with administration of potassium-depleting diuretics, increasing the potential for Torsade de Pointes. Potassium levels should be within the normal range prior to administration of TIKOSYN and maintained in the normal range during administration of TIKOSYN (see DOSAGE AND ADMINISTRATION).
The use of TIKOSYN in conjunction with other drugs that prolong the QT interval has not been studied and is not recommended. Such drugs include phenothiazines, cisapride, bepridil, tricyclic antidepressants, certain oral macrolides, and certain fluoroquinolones. Class I or Class III antiarrhythmic agents should be withheld for at least three half-lives prior to dosing with TIKOSYN. In clinical trials, TIKOSYN was administered to patients previously treated with oral amiodarone only if serum amiodarone levels were below 0.3 mg/L or amiodarone had been withdrawn for at least three months.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
TIKOSYN is indicated for the maintenance of normal sinus rhythm (delay in time to recurrence of atrial fibrillation/atrial flutter [AF/AFl]) in patients with atrial fibrillation/atrial flutter of greater than one week duration who have been converted to normal sinus rhythm. Because TIKOSYN can cause life threatening ventricular arrhythmias, it should be reserved for patients in whom atrial fibrillation/atrial flutter is highly symptomatic.
In general, antiarrhythmic therapy for atrial fibrillation/atrial flutter aims to prolong the time in normal sinus rhythm. Recurrence is expected in some patients (see CLINICAL STUDIES).
TIKOSYN is indicated for the conversion of atrial fibrillation and atrial flutter to normal sinus rhythm.
TIKOSYN has not been shown to be effective in patients with paroxysmal atrial fibrillation.
History
There is currently no drug history available for this drug.
Other Information
TIKOSYN® (dofetilide) is an antiarrhythmic drug with Class III (cardiac action potential duration prolonging) properties. Its empirical formula is C19H27N3O5S2 and it has a molecular weight of 441.6. The structural formula is

The chemical name for dofetilide is:
N-[4-[2-[methyl[2-[4-[(methylsulfonyl)amino]phenoxy]ethyl]amino]ethyl]phenyl]-methanesulfonamide.
Dofetilide is a white to off-white powder. It is very slightly soluble in water and propan-2-ol and is soluble in 0.1M aqueous sodium hydroxide, acetone, and aqueous 0.1M hydrochloric acid.
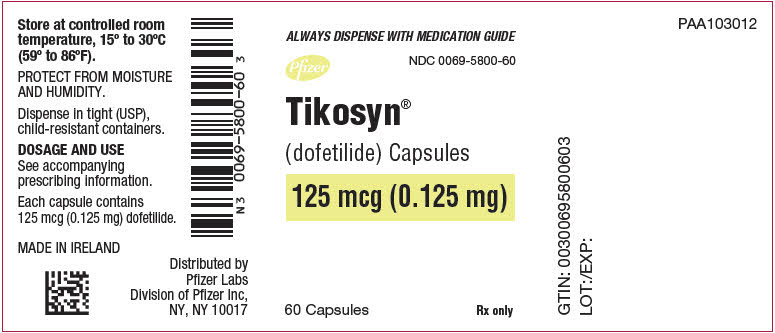
TIKOSYN capsules contain the following inactive ingredients: microcrystalline cellulose, corn starch, colloidal silicon dioxide and magnesium stearate. TIKOSYN is supplied for oral administration in three dosage strengths: 125 mcg (0.125 mg) orange and white capsules, 250 mcg (0.25 mg) peach capsules, and 500 mcg (0.5 mg) peach and white capsules.
Sources
Tikosyn Manufacturers
-
Pfizer Laboratories Div Pfizer Inc
![Tikosyn (Dofetilide) Capsule [Pfizer Laboratories Div Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Tikosyn | Pfizer Laboratories Div Pfizer Inc
![Tikosyn (Dofetilide) Capsule [Pfizer Laboratories Div Pfizer Inc] Tikosyn (Dofetilide) Capsule [Pfizer Laboratories Div Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Therapy with TIKOSYN must be initiated (and, if necessary, re-initiated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of three days. Additionally, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm. The dose of TIKOSYN must be individualized according to calculated creatinine clearance and QTc. (QT interval should be used if the heart rate is <60 beats per minute. There are no data on use of TIKOSYN when the heart rate is <50 beats per minute.) The usual recommended dose of TIKOSYN is 500 mcg BID, as modified by the dosing algorithm described below. For consideration of a lower dose, see Special Considerations below. Serum potassium should be maintained within the normal range before TIKOSYN treatment is initiated and should be maintained within the normal range while the patient remains on TIKOSYN therapy. (See WARNINGS, Hypokalemia and Potassium-Depleting Diuretics). In clinical trials, potassium levels were generally maintained above 3.6–4.0 mEq/L. Patients with atrial fibrillation should be anticoagulated according to usual medical practice prior to electrical or pharmacological cardioversion. Anticoagulant therapy may be continued after cardioversion according to usual medical practice for the treatment of people with AF. Hypokalemia should be corrected before initiation of TIKOSYN therapy (see WARNINGS, Ventricular Arrhythmia). Patients to be discharged on TIKOSYN therapy from an inpatient setting as described above must have an adequate supply of TIKOSYN, at the patient's individualized dose, to allow uninterrupted dosing until the patient receives the first outpatient supply. TIKOSYN is distributed only to those hospitals and other appropriate institutions confirmed to have received applicable dosing and treatment initiation education programs. Inpatient and subsequent outpatient discharge and refill prescriptions are filled only upon confirmation that the prescribing physician has received applicable dosing and treatment initiation education programs. For this purpose, a list for use by pharmacists is maintained containing hospitals and physicians who have received one of the education programs. Instructions for Individualized Dose Initiation Initiation of TIKOSYN TherapyStep 1. Electrocardiographic assessment: Prior to administration of the first dose, the QTc must be determined using an average of 5–10 beats. If the QTc is greater than 440 msec (500 msec in patients with ventricular conduction abnormalities), TIKOSYN is contraindicated. If heart rate is less than 60 beats per minute, QT interval should be used. Patients with heart rates <50 beats per minute have not been studied.
Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance must be calculated using the following formula:
creatinine clearance (male) = (140-age) × actual body weight in kg
72 × serum creatinine (mg/dL) creatinine clearance (female) = (140-age) × actual body weight in kg × 0.85
72 × serum creatinine (mg/dL)When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L).
Step 3. Starting Dose: The starting dose of TIKOSYN is determined as follows:
Calculated Creatinine Clearance TIKOSYN Dose >60 mL/min 500 mcg twice daily 40 – 60 mL/min 250 mcg twice daily 20 – <40 mL/min 125 mcg twice daily <20 mL/min Dofetilide is contraindicated
in these patientsStep 4. Administer the adjusted TIKOSYN dose and begin continuous ECG monitoring.
Step 5. At 2–3 hours after administering the first dose of TIKOSYN, determine the QTc. If the QTc has increased by greater than 15% compared to the baseline established in Step 1 OR if the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), subsequent dosing should be adjusted as follows:
If the Starting Dose Based on
Creatinine Clearance is: Then the Adjusted Dose
(for QTc Prolongation) is: 500 mcg twice daily 250 mcg twice daily 250 mcg twice daily 125 mcg twice daily 125 mcg twice daily 125 mcg once a dayStep 6. At 2–3 hours after each subsequent dose of TIKOSYN, determine the QTc (for in-hospital doses 2–5). No further down titration of TIKOSYN based on QTc is recommended.
NOTE: If at any time after the second dose of TIKOSYN is given the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), TIKOSYN should be discontinued.
Step 7. Patients are to be continuously monitored by ECG for a minimum of three days, or for a minimum of 12 hours after electrical or pharmacological conversion to normal sinus rhythm, whichever is greater.
The steps described above are summarized in the following diagram:
Maintenance of TIKOSYN TherapyRenal function and QTc should be re-evaluated every three months or as medically warranted. If QTc exceeds 500 milliseconds (550 msec in patients with ventricular conduction abnormalities), TIKOSYN therapy should be discontinued and patients should be carefully monitored until QTc returns to baseline levels. If renal function deteriorates, adjust dose as described in Initiation of TIKOSYN Therapy, Step 3.
Special Considerations Consideration of a Dose Lower than that Determined by the AlgorithmThe dosing algorithm shown above should be used to determine the individualized dose of TIKOSYN. In clinical trials (see CLINICAL STUDIES), the highest dose of 500 mcg BID of TIKOSYN as modified by the dosing algorithm led to greater effectiveness than lower doses of 125 or 250 mcg BID as modified by the dosing algorithm. The risk of Torsade de Pointes, however, is related to dose as well as to patient characteristics (see WARNINGS). Physicians, in consultation with their patients, may therefore in some cases choose doses lower than determined by the algorithm. It is critically important that if at any time this lower dose is increased, the patient needs to be rehospitalized for three days. Previous toleration of higher doses does not eliminate the need for rehospitalization.
The maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 500 mcg BID; doses greater than 500 mcg BID have been associated with an increased incidence of Torsade de Pointes.
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
CardioversionIf patients do not convert to normal sinus rhythm within 24 hours of initiation of TIKOSYN therapy, electrical conversion should be considered. Patients continuing on TIKOSYN after successful electrical cardioversion should continue to be monitored by electrocardiography for 12 hours post cardioversion, or a minimum of 3 days after initiation of TIKOSYN therapy, whichever is greater.
Switch to TIKOSYN from Class I or other Class III Antiarrhythmic TherapyBefore initiating TIKOSYN therapy, previous antiarrhythmic therapy should be withdrawn under careful monitoring for a minimum of three (3) plasma half-lives. Because of the unpredictable pharmacokinetics of amiodarone, TIKOSYN should not be initiated following amiodarone therapy until amiodarone plasma levels are below 0.3 mcg/mL or until amiodarone has been withdrawn for at least three months.
Stopping TIKOSYN Prior to Administration of Potentially Interacting DrugsIf TIKOSYN needs to be discontinued to allow dosing of other potentially interacting drug(s), a washout period of at least two days should be followed before starting the other drug(s).
Login To Your Free Account