FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Wellbutrin Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
There is currently no warning information available for this product. We apologize for any inconvenience.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
WELLBUTRIN (bupropion hydrochloride)is indicated for the treatment of major depressive disorder(MDD), as defined by the Diagnostic and Statistical Manual (DSM).
The efficacy of WELLBUTRIN in the treatment of a major depressive episode was established in two 4-week controlled inpatient trials and one 6-week controlled outpatient trial of adult subjects with MDD [see Clinical Studies (14)].
History
There is currently no drug history available for this drug.
Other Information
WELLBUTRIN (bupropion hydrochloride), an antidepressant of the aminoketone class, is chemically unrelated to tricyclic, tetracyclic, selective serotonin re‑uptake inhibitor, or other known antidepressant agents. Its structure closely resembles that of diethylpropion; it is related to phenylethylamines. It is designated as (±)-1-(3-chlorophenyl)-2-[(1,1-dimethylethyl)amino]-1-propanone hydrochloride. The molecular weight is 276.2. The molecular formula is C13H18ClNO•HCl. Bupropion hydrochloride powder is white, crystalline, and highly soluble in water. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. The structural formula is:

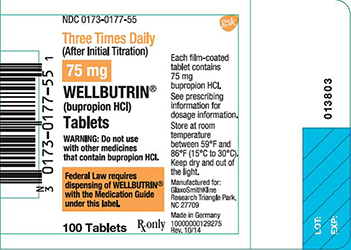
WELLBUTRIN is supplied for oral administration as 75‑mg (yellow‑gold) and 100‑mg (red) film‑coated tablets. Each tablet contains the labeled amount of bupropion hydrochloride and the inactive ingredients: 75‑mg tablet – D&C Yellow No. 10 Lake, FD&C Yellow No. 6 Lake, hydroxypropyl cellulose, hypromellose, microcrystalline cellulose, polyethylene glycol, talc, and titanium dioxide; 100‑mg tablet – FD&C Red No. 40 Lake, FD&C Yellow No. 6 Lake, hydroxypropyl cellulose, hypromellose, microcrystalline cellulose, polyethylene glycol, talc, and titanium dioxide.
Sources
Wellbutrin Manufacturers
-
Remedyrepack Inc.
![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Wellbutrin | Remedyrepack Inc.
![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Remedyrepack Inc. ] Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
•Starting Dose: 200 mg per day given as 100 mg twice daily (2.1)•General: Increase dose gradually to reduce seizure risk. (2.1, 5.3)•After 3 days, may increase the dose to 300 mg per day, given as 100 mg 3 times daily at an interval of at least 6 hours between doses. (2.1) •Usual target dose: 300 mg per day as 100 mg 3 times daily. (2.1) •Maximum dose: 450 mg per day given as 150 mg 3 times daily. (2.1) •Periodically reassess the dose and need for maintenance treatment. (2.1)•Moderate to severe hepatic impairment: 75 mg once daily. (2.2, 8.7) •Mild hepatic impairment: Consider reducing the dose and/or frequency of dosing. (2.2, 8.7)•Renal Impairment: Consider reducing the dose and/or frequency. (2.3, 8.6)
To minimize the risk of seizure, increase the dose gradually [see Warnings and Precautions (5.3)]. Increases in dose should not exceed 100 mg per day in a 3‑day period. WELLBUTRIN Tablets should be swallowed whole and not crushed, divided, or chewed. WELLBUTRIN may be taken with or without food.
The recommended starting dose is 200 mg per day, given as 100 mg twice daily. After 3 days of dosing, the dose may be increased to 300 mg per day, given as 100 mg 3 times daily, with at least 6 hours between successive doses. Dosing above 300 mg per day may be accomplished using the 75- or 100-mg tablets.
A maximum of 450 mg per day, given in divided doses of not more than 150 mg each, may be considered for patients who show no clinical improvement after several weeks of treatment at 300 mg per day. Administer the 100‑mg tablet 4 times daily to not exceed the limit of 150 mg in a single dose.
It is generally agreed that acute episodes of depression require several months or longer of antidepressant drug treatment beyond the response in the acute episode. It is unknown whether the dose of WELLBUTRIN needed for maintenance treatment is identical to the dose that provided an initial response. Periodically reassess the need for maintenance treatment and the appropriate dose for such treatment.
In patients with moderate to severe hepatic impairment (Child-Pugh score: 7 to15), the maximum dose of WELLBUTRIN is 75 mg per day. In patients with mild hepatic impairment (Child-Pugh score: 5 to 6), consider reducing the dose and/or frequency of dosing [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
Consider reducing the dose and/or frequency of WELLBUTRIN in patients with renal impairment (Glomerular Filtration Rate <90 mL/min) [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of therapy with WELLBUTRIN. Conversely, at least 14 days should be allowed after stopping WELLBUTRIN before starting an MAOI antidepressant [see Contraindications (4) and Drug Interactions (7.6)].
Do not start WELLBUTRIN in a patient who is being treated with a reversible MAOI such as linezolid or intravenous methylene blue. Drug interactions can increase the risk of hypertensive reactions. In a patient who requires more urgent treatment of a psychiatric condition, non-pharmacological interventions, including hospitalization, should be considered [see Contraindications (4) and Drug Interactions (7.6)].
In some cases, a patient already receiving therapy with WELLBUTRIN may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of hypertensive reactions in a particular patient, WELLBUTRIN should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with WELLBUTRIN may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue.
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with WELLBUTRIN is unclear. The clinician should, nevertheless, be aware of the possibility of a drug interaction with such use [see Contraindications (4) and Drug Interactions (7.6)].
-
Glaxosmithkline Llc
![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Glaxosmithkline Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Wellbutrin | Glaxosmithkline Llc
![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Glaxosmithkline Llc] Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Glaxosmithkline Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Instructions for UseTo minimize the risk of seizure, increase the dose gradually [see Warnings and Precautions (5.3)]. Increases in dose should not exceed 100 mg per day in a 3‑day period. WELLBUTRIN Tablets should be swallowed whole and not crushed, divided, or chewed. WELLBUTRIN may be taken with or without food.
The recommended starting dose is 200 mg per day, given as 100 mg twice daily. After 3 days of dosing, the dose may be increased to 300 mg per day, given as 100 mg 3 times daily, with at least 6 hours between successive doses. Dosing above 300 mg per day may be accomplished using the 75- or 100-mg tablets.
A maximum of 450 mg per day, given in divided doses of not more than 150 mg each, may be considered for patients who show no clinical improvement after several weeks of treatment at 300 mg per day. Administer the 100‑mg tablet 4 times daily to not exceed the limit of 150 mg in a single dose.
It is generally agreed that acute episodes of depression require several months or longer of antidepressant drug treatment beyond the response in the acute episode. It is unknown whether the dose of WELLBUTRIN needed for maintenance treatment is identical to the dose that provided an initial response. Periodically reassess the need for maintenance treatment and the appropriate dose for such treatment.
2.2 Dose Adjustment in Patients with Hepatic ImpairmentIn patients with moderate to severe hepatic impairment (Child-Pugh score: 7 to 15), the maximum dose of WELLBUTRIN is 75 mg per day. In patients with mild hepatic impairment (Child-Pugh score: 5 to 6), consider reducing the dose and/or frequency of dosing [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)].
2.3 Dose Adjustment in Patients with Renal ImpairmentConsider reducing the dose and/or frequency of WELLBUTRIN in patients with renal impairment (Glomerular Filtration Rate <90 mL/min) [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.4 Switching a Patient to or from a Monoamine Oxidase Inhibitor (MAOI) AntidepressantAt least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of therapy with WELLBUTRIN. Conversely, at least 14 days should be allowed after stopping WELLBUTRIN before starting an MAOI antidepressant [see Contraindications (4), Drug Interactions (7.6)].
2.5 Use of WELLBUTRIN with Reversible MAOIs Such as Linezolid or Methylene BlueDo not start WELLBUTRIN in a patient who is being treated with a reversible MAOI such as linezolid or intravenous methylene blue. Drug interactions can increase the risk of hypertensive reactions. In a patient who requires more urgent treatment of a psychiatric condition, non-pharmacological interventions, including hospitalization, should be considered [see Contraindications (4), Drug Interactions (7.6)].
In some cases, a patient already receiving therapy with WELLBUTRIN may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of hypertensive reactions in a particular patient, WELLBUTRIN should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with WELLBUTRIN may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue.
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with WELLBUTRIN is unclear. The clinician should, nevertheless, be aware of the possibility of a drug interaction with such use [see Contraindications (4), Drug Interactions (7.6)].
Login To Your Free Account


![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=fb118c90-41b7-4bc9-a82f-a4a415faabbb&name=MM2.jpg)
![Wellbutrin (Bupropion Hydrochloride) Tablet, Film Coated [Glaxosmithkline Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=60525754-0d2b-4ba4-918a-1c9d3eff89b2&name=wellbutrin-spl-graphic-02.jpg)